Pilex
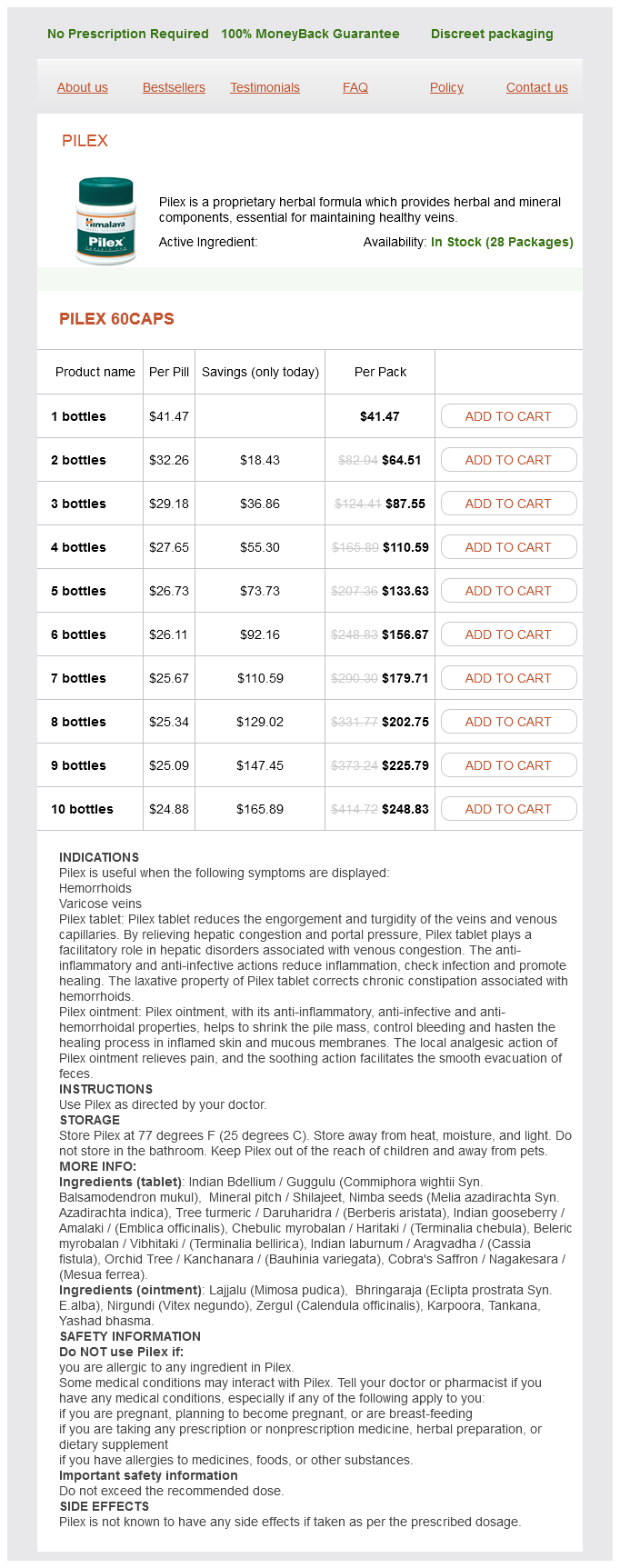
Pilex 60caps
- 1 bottles - $41.47
- 2 bottles - $64.51
- 3 bottles - $87.55
- 4 bottles - $110.59
- 5 bottles - $133.63
- 6 bottles - $156.67
- 7 bottles - $179.71
- 8 bottles - $202.75
- 9 bottles - $225.79
- 10 bottles - $248.83
To link in vitro and in vivo studies prostate antigen 60 caps pilex order overnight delivery, several authors have suggested using extrapolation techniques, based on the comparison of in vitro inhibition data with the active in vivo concentrations of the inhibitor. However, the lack of knowledge with regard to one or several important parameters, such as the role of metabolites and intrahepatocyte accumulation, often limits the ability to make safe and accurate predictions. The uncertainty and inaccuracy of predicting the extent and duration of in vivo drug interactions currently stems from a lack of definitive models by which to assess likely substrate and inhibitor concentrations at the active site of metabolism. Additional issues contributing to the uncertainty of predicting drug interactions include assumptions of the contribution of presystemic drug extraction and the effect of inhibitors on the processes involved. As a consequence, these methods are useful for complementing in vivo studies and helping to design clinically relevant in vivo studies, but in the foreseeable future they will not totally replace in vivo investigations. Available evidence indicates that the risk of this combination is considerably greater in patients receiving high-dose methotrexate as cancer chemotherapy than it is in patients receiving lower weekly dosages for psoriasis20. This is because the distribution of the drug is not very important mechanistically in determining drug interactions, but changes in drug elimination are. Gender-related differences in pharmacokinetics may cause variations in drug absorption, gastric emptying, and distribution based on percentage of adipose tissue21. More specifically, clinically significant interactions occur more frequently with drugs that have a narrow margin of safety, i. Drugs with the potential for such serious interactions include warfarin and cyclosporine. Medication-related factors that contribute to clinical risk include the dose, route of administration and duration of administration of the precipitant drug (the drug that causes the interaction) as well as the sequence of administration of the interacting drugs. That is, as the dose of the precipitant drug is increased, the magnitude of its effect on the object drug tends to increase. However, the dose of the object drug may also affect the risk of an adverse drug interaction. For example, a patient who takes small doses of an object drug with serum concentrations at the lower end of the target range is at a lesser risk when an enzymeinhibiting precipitant drug is added, than would be a patient taking large doses of the same object drug. This reduces the bioavailability or the amount of drug available to the systemic circulation and results in subtherapeutic serum concentrations. Common drugs that form complexes with other drugs include antacids, sucralfate, and bile acid sequestrants. A significant interaction occurs between multivalent cations such as calcium, aluminum, iron and magnesium and tetracyclines or fluoroquinolone antibiotics. The bound substrate drug is excreted in the feces, thereby effectively shortening its half-life. An example of this is the concurrent administration of warfarin and bile acid sequestrants. These transporters are found in multiple tissues and actively pump drug molecules either out of cells (efflux) or into cells (uptake). An understanding of the physiologic regulation of these transporter proteins is key to designing strategies for improving the therapeutic efficacy of drugs that serve as their substrates (Table 131. These membrane-bound transport systems appear to have developed as a mechanism for protecting the body from harmful substances. These interactions can be easily avoided by administering the fluoroquinolone at least 2 hours before or 6 hours after the antacid or iron. Alendronate, as well as other bisphosphonates prescribed for the prevention and treatment of osteoporosis, forms complexes with cations and several other drugs, thereby further decreasing their already low oral absorption. Once-weekly dosing reduces the opportunity for bisphosphonate-related interactions. Drugs that increase gastric pH, such as proton pump inhibitors, antacids and H2 antihistamines, may reduce the absorption of drugs such as itraconazole, posaconazole and ketoconazole, which are best absorbed in an acidic environment27. Although itraconazole is best absorbed when the gastric pH is low, its administration with food is more important for achieving high plasma concentrations28. Similarly, the coadministration of drugs that can increase gastric pH (see above) with atazanavir and raltegravir are not recommended. Some drugs may interfere with the enterohepatic recirculation of a substrate drug. When one drug displaces another from plasma protein-binding sites, the free serum concentration of the displaced drug is increased and its pharmacologic effect increases.
Pilex dosages: 60 capsPilex packs: 1 bottles, 2 bottles, 3 bottles, 4 bottles, 5 bottles, 6 bottles, 7 bottles, 8 bottles, 9 bottles, 10 bottles
Pathogenesis A nasal glioma is the result of embryologic displacement of brain tissue androgen hormone joint cheap pilex 60 caps fast delivery, usually along the cranial closure lines and without apparent communication with underlying structures83. It has a predilection for the perinasal area; therefore, it is commonly referred to as a nasal glioma. Clinical features Nasal gliomas are firm, smooth-surfaced, skin-colored to redviolet papulonodules that may have obvious telangiectasias and range in size from 1 to 3 cm. Pathology In a nasal glioma, an ill-defined, non-encapsulated neuropil-like mass is seen within the dermis and subcutis. The neuropil-like tissue is composed of nests and strands of pale-staining, finely vacuolated or fibrillary matrix in which various types of astrocytes can be found83. Gemistocytic astrocytes, with polygonal, eosinophilic cytoplasm and eccentric nuclei, as well as multinucleated giant cells, are relatively common. Occasionally, residual meningoendothelial cells, ependymal cells, choroid plexuslike structures, and pigmented cells can be identified85. Differential diagnosis Clinically, the lesion must be differentiated from other facial midline lesions (see Ch. Treatment Most cutaneous neural malformations can be effectively treated by excision. Cranial imaging is recommended before these lesions are biopsied or removed87, because nasal gliomas can communicate with the intracranial space, and therefore cerebrospinal fluid leakage and subsequent meningoencephalitis and other neurologic damage may occur after biopsy84. Epidemiology Meningeal heterotopias are rare lesions, usually apparent at or shortly after birth88. Sentinel lymph node biopsy for evaluation and treatment of patients with Merkel cell carcinoma: the Dana-Farber experience and meta-analysis of the literature. Although these lesions are sometimes classified as type I cutaneous meningiomas88, considering their non-neoplastic nature, they are better classified as rudimentary meningoceles89. Clinical features Rudimentary meningoceles most commonly present on the scalp of neonates and infants at the sites of cranial closure. Skin-colored papules or nodules on the scalp are often associated with alopecia and/ or the "hair collar" sign90. Pathology 2064 A rudimentary meningocele is an ill-defined mass of cavernous, pseudovascular spaces embedded in a markedly collagenous stroma89,91. The spaces may be lined by elongated meningoendothelial cells characterized by eosinophilic cytoplasm, round or ovoid nuclei, and a fine Differential diagnosis In neonates and infants, rudimentary meningoceles must be distinguished from "atretic" meningoceles (an intermediate form with an intracranial connection), membranous aplasia cutis congenita, heterotopic brain tissue, dermoid cysts, and infantile hemangiomas. Within the deep dermis or subcutis, there is a multinodular mass, often with an infiltrative growth pattern9395. The cells may show a variable degree of differentiation, and in the most common form, the spindle cells have a concentric, whorl-like arrangement93; psammoma bodies are often present9395. Clinically, these nodular tumors may have associated alopecia and can resemble an epidermoid or pilar cyst, adnexal tumor or cutaneous metastasis. More recently, studies have implicated the anaplastic lymphoma kinase gene in the tumorigenesis of many familial and some sporadic cases of neuroblastoma. Clinical Features In children, the cutaneous metastases of neuroblastoma often manifest as multiple, blue to purple, dermal papules or nodules that resemble the "blueberry muffin" lesions seen with congenital infections or hematologic disorders4 (see Ch. Treatment As with heterotopic neuroglial tissue (nasal glioma), imaging studies are required prior to biopsy or excision. The tumor mass is composed of atypical, small, dark cells with scant cytoplasm3,97. The cells have larger nuclei than mature lymphocytes (with a coarse chromatin pattern) and they form irregular nests, cords, or poorly cohesive sheets. Rosette formation, by concentrically arranged tumor cells in double or multiple circles, is common. They display a wide spectrum of clinicopathologic features based on their relative degree of differentiation, ranging from very primitive neuroectodermal tumors to more mature forms such as neuroblastomas. Since then, different terms have been used for tumors with cytologically similar features, reflecting the controversy regarding this entity. Similar cells dissect or wrap around collagen fibers, producing "collagen bodies". Focal calcification and psammoma bodies (eosinophilic laminated and whorled structures with variable calcification) may occur.
Einbeere (Herb Paris). Pilex.
- How does Herb Paris work?
- What is Herb Paris?
- Headache; living longer; nerve pain; sore and painful muscles and joints; genital tumors; rapid fluttering or throbbing of the heart; muscle spasms; use as a medicine to cause vomiting, or cleansing and emptying the intestinal tract.
- Dosing considerations for Herb Paris.
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96200
Therefore prostate 8-k run eugene oregon cheap 60 caps pilex, the primary movement of a flap creates a primary tension vector, while the secondary movement (during closure of the donor site defect) creates a secondary tension vector. Consideration of these forces and the effects of these forces on adjacent tissue and even the blood supply of the flap is the primary factor in selecting one flap over another7. The most perfectly executed flap that, via tension vectors, results in the distortion of a free margin. Therefore, the initial and most important skill required for the proper execution of flaps is the ability to anticipate the direction and amount of tension created by particular flaps and to predict what effects this tension will have on adjacent structures. There are four broad categories of flaps based upon how the tissue is rearranged in order to achieve closure (Table 147. The second includes the flaps that reconfigure defects, while the third includes flaps that reorient tissue from adjacent pools of laxity into the defect. Finally, there is a category of flaps that enables defect closure by tissue importation. Movement of this flap is entirely dependent on the elasticity of the tissue that comprises the flap. Tissue reorientation flaps Tissue reorientation flaps are characterized by the lifting of skin from an adjacent donor site and reorienting it through the transposition of the flap over a peninsula of skin between the donor site and the defect. Although intrinsic elasticity of the flap skin may facilitate the ease of execution, without ample laxity in the donor site, the transposition cannot be performed. Some of the flaps that fall into this category include the rhombic transposition flap, the bilobed transposition flap, and the nasolabial transposition flap (see Table 147. To better understand the reorientation of tissue that occurs in these flaps, a review of the most basic tissue reorientation flap, the Z-plasty, is helpful. There is a complementary decrease in the length of skin perpendicular to this same arm. Put another way, tissue gain in the direction of the middle arm is proportional to the width of the base of the flaps. Therefore, just as with Z-plasties, transposition flaps work because the reorientation of the tissue results in lengthening of tissue in the direction of the skin deficit at the expense of the laxity in the donor site. The skin is typically very tight in this area, making simple side-to-side closure in the vertical direction difficult. Side-to-side closure in the horizontal direction is impractical because of the distortion that would occur to the free margin of the ala. When one looks for donor sites, there is typically a substantial amount of laxity on the mid nasal dorsum and nasal sidewall. A bilobed flap allows utilization of this laxity through tissue reorientation using two lobes9. The underlying mechanism of tissue reorientation is a series of Z-plasties inherent in this flap. Since tissue gain in Z-plasties is in the direction of the middle arm of the Z-plasty, a substantial reorientation and lengthening of tissue in the desirable direction for repair of the defect occurs without distortion10. When the surrounding skin is elastic and "loose", the wound edges can be closed under minimal tension in both a side-to-side closure and with these flaps. Thus, the only advantage that these flaps confer over a side-to-side closure in tight skin is that a larger area of skin is typically undermined, which releases the flap from the tethering effect of the subcutaneous tissue. Tissue importation flaps Large defects, or defects in areas where tissue laxity is lacking, may be reconstructed by importing vascularized skin from a site that is not adjacent to the defect (see Table 147. Tissue importation flaps are typically derived from a distant donor site with ample tissue laxity and, most importantly, an excellent blood supply. These flaps are typically two-staged flaps requiring a period of vascular ingrowth from the wound bed of the defect. This time period ranges from 2 to 6 weeks, with 3 weeks being the most commonly reported time point for transection of the pedicle. In the head and neck region, defect sites where tissue importation flaps are commonly employed include the nose, ear, eyelid, and lip.
Syndromes
- Brain and nervous system infections, such as meningitis, myelitis, and encephalitis
- Do not tackle or dive into a person with your head.
- Your doctor or nurse will tell you when to arrive.
- Kidney disease or dialysis (you may not be able to receive contrast)
- School problems
- Corticosteroids
- Meningitis - staphylococcal
Marking can be done according to the custom of the surgeon mens health yoga workout order genuine pilex line, but should be devised so that the subsequent distortion by local anesthetic infiltration will not obscure the various thicknesses of the adiposity. Existing dimples and dents should also be outlined for later identification during surgery so that they can be avoided. If significant sedation is to be employed, peripheral venous catheters and monitoring devices such as pulse oximeters and cardiac monitors can be utilized. While patients undergoing the tumescent technique usually require very little ancillary sedation, most patients do appreciate pre-sedation with mild oral sedatives such as lorazepam. Those who are pain-sensitive can receive minor additional sedation such as 25 mg of meperidine intramuscularly, a dose which does not impair protective reflexes. Of note, more aggressive forms of systemic anesthesia and rapid infiltration are associated with an increased potential for abdominal perforation. Deeply sedated patients may not even complain of the discomfort associated with muscular penetration. Another disadvantage of moderate and deep sedation is that because of concerns about total anesthesia time, there is usually little or no delay between infiltration of the tumescent fluid and the beginning of the procedure. As noted previously, significant vasoconstriction from the infiltration of the tumescent fluid does not occur for at least 1015 minutes after infiltration. Liposuction can be performed using many different types of cannulas and aspirators. The number of holes arranged along the shaft of the cannula is probably unimportant, although two or more holes increase the flow of fat through the instrument. The most important parameter for choosing cannulas is size: the smallest possible cannula should be employed. Also smaller-diameter cannulas penetrate the fat more easily and create less tissue trauma. Longer cannulas allow the surgeon to work from fewer skin insertion sites, leaving fewer scars whereas shorter cannulas are easier to control as they pass through subcutaneous tissue. The tiny incisions required for insertion of 3 mm cannulas leave nearly invisible scars in most patients, but can be an issue if the patient has a tendency towards keloids or hyperpigmentation. Liposuction is based on the technique of criss-crossing tunnels (from multiple insertion sites) through the subcutaneous tissue. Each area to be suctioned should be tunneled from at least two different directions, but often three or four are more effective. Multiple small tunnels ultimately provide the smoothest contraction of the overlying skin and the most thorough removal of fat. A red aspirate in the suction tubing indicates excessive bleeding and the surgeon should immediately move on to a different tunnel. At the same time, the free hand pulls, presses and squeezes the skin to facilitate penetration of the cannula; it also provides important tactile information about the thickness of the underlying fat. The final surgical endpoint should be a skin thickness in the suctioned areas which is similar to that of the surrounding non-treated skin. Experience has shown that closing insertion sites with sutures leads to a greater increase in postoperative edema as well as more bruising due to decreased postoperative drainage. The authors generally prefer to use a #15c blade to create insertion sites because this leads to less visible scarring. Klein17 has advocated the creation of 12 mm openings with a punch biopsy instrument. The latter are more likely to stay open during the initial postoperative period, but may leave more noticeable scars. On the other hand, bupivacaine is contraindicated for tumescent liposuction because bupivacaineassociated cardiac toxicity can be subtle, is not preceded by convulsions, and is often unresponsive to resuscitation24. In Europe, prilocaine has been used instead of lidocaine for tumescent anesthesia25. Typical,nearlybloodless liposuctionaspirate usingthetumescent technique of fat, when compared to manual cannulas, but retain some feel of tissue resistance29.
Usage: gtt.
Under local anesthesia mens health institute order generic pilex, specimens may be obtained via a number of different surgical procedures including curettage, punch biopsy, shave or saucerization excision, incisional sampling, and excision in toto. The wounds then heal by second intention or by a layered closure with initial suturing of the subcutaneous tissue followed by suturing of the epidermis. Contraindications are few although modifications may be required to deal with patient or anatomic site issues. Likewise, complications are few and are generally preventable with appropriate aftercare. The volume of tissue sampled correlates with the size of the punch biopsy instrument. In general, the diameter of the metal "barrel" varies from 2 to 6 mm, and the wider the diameter, the greater the likelihood of obtaining subcutaneous fat. However, the thickness of the dermis and the amount of subcutaneous fat required to establish the diagnosis must be kept in mind. Punch biopsies are particularly helpful for examining processes within the dermis. In the case of tumors, sampling a majority of the lesion is desirable, so that for large-sized tumors, multiple punch biopsies may be required. The incisional biopsy removes a wedge of tissue from the center or edge of a lesion (see Site selection) and is the best option for obtaining deep subcutaneous fat or fascia for histologic examination. Excision in toto removes the entire lesion and includes epidermis, dermis and subcutaneous fat. For these reasons, it is often utilized when the leading clinical diagnosis is invasive cutaneous melanoma. Most specimens are placed in formalin, but, occasionally, special carrier media are necessary (Table 146. Fresh tissue specimens are sent on salinemoistened gauze and either promptly delivered to the laboratory or packed in ice; the laboratory must be in reasonable proximity and have the capability of processing the tissue immediately. When handling small or thin biopsy specimens, it is important to confirm that they are clearly within the formalin solution and not adhering to the upper portions of the container or lid; this prevents desiccation artifact. If multiple biopsies are to be performed, pre-labeling the containers alphabetically and with the respective sites avoids confusion. Culture for viruses Electron microscopy *Laboratory must be in close proximity and specimen placed on saline-moistened gauze, but need to avoid bacteriostatic saline solution when culturing for microbes. Informed consent requires a discussion of the major risks, which include bleeding, discomfort, infection, and scarring (see Ch. Bleeding can usually be controlled by firm pressure at the site of the wound, but may require more aggressive forms of hemostasis. Discomfort is usually minimal, although some sites such as the forehead, fingers and feet may throb. Except when the area to be biopsied is already infected or the site is mucosal, the skin can be prepared by application of an antiseptic agent and the procedure is then considered to be a clean procedure. For clean procedures of non-mucosal, non-infected sites, preoperative prophylactic antibiotics are currently not recommended, even in patients with artificial valves or joints (with the possible exception of sites at high risk of infection. The overall goal is a reduction in the emergence of antibiotic-resistant bacteria and in one study, for example, preoperative prophylactic antibiotics increased nasal carriage of methicillin-resistant Staphylococcus aureus5. Preoperative antibiotics are administered within a 2-hour window before the incision; there is debate as to whether or not a second dose is administered 6 hours later and under which circumstances antibiotics should be continued for 4872 hours6. When pretreated with a 5-day regimen of intranasal mupirocin ointment (twice daily) and a total body wash with chlorhexidine soap (daily avoiding the eyes and ears), nasal carriers of S. Most patients are primarily interested in discussing whether or not there will be visible scarring. This is best predicted by the type of biopsy to be performed and the anatomic site. Generally, patients can be reassured that small biopsies may be done without grossly noticeable permanent "marks". Many patients are anxious about the needle sticks required for administration of the local anesthesia and the pain of the procedure. A well-informed, comfortable patient in a supine position will tolerate the procedure without difficulty.
References
- Koob GF, Le Moal M. Drug addiction, dysregulation of reward, and allostasis. Neuropsychopharmacol. 2001;24:97-129.
- Azzimondi G, Bassein L, Nonino F, et al: Fever in acute stroke worsens prognosis: a prospective study, Stroke 26:2040-2043, 1995.
- Oosterlinck W, Kurth KH, Schroder F, et al: A prospective European Organization for Research and Treatment of Cancer Genitourinary Group randomized trial comparing transurethral resection followed by a single intravesical instillation of epirubicin or water in single state Ta, T1 papillary carcinoma of the bladder, J Urol 149:749n752, 1993.
- Dooley RE, Pietrow PK: Ureteroscopy for benign hematuria, Urol Clin North Am 31:137-143, 2004.
- Paglioli E, Palmini A, Portuguez M et al. Seizure and memory outcome following temporal lobe surgery: selective compared with nonselective approaches for hippocampal sclerosis. J Neurosurg 104(1): 70-78, 2006.