Lamotrigine
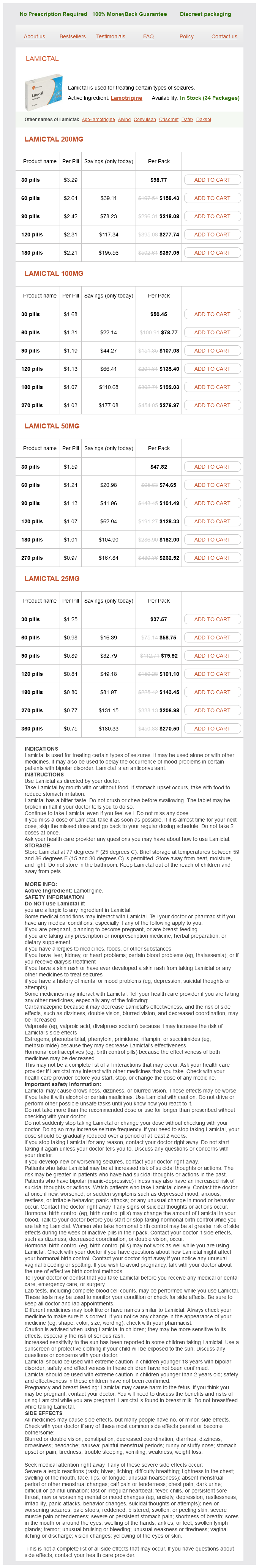
Lamictal 200mg
- 30 pills - $98.77
- 60 pills - $158.43
- 90 pills - $218.08
- 120 pills - $277.74
- 180 pills - $397.05
Lamictal 100mg
- 30 pills - $50.45
- 60 pills - $78.77
- 90 pills - $107.08
- 120 pills - $135.40
- 180 pills - $192.03
- 270 pills - $276.97
Lamictal 50mg
- 30 pills - $47.82
- 60 pills - $74.65
- 90 pills - $101.49
- 120 pills - $128.33
- 180 pills - $182.00
- 270 pills - $262.52
Lamictal 25mg
- 30 pills - $37.57
- 60 pills - $58.75
- 90 pills - $79.92
- 120 pills - $101.10
- 180 pills - $143.45
- 270 pills - $206.98
- 360 pills - $270.50
Erythematous papules have coalesced to form a plaque on the right cheek treatment 2 order lamotrigine no prescription, V of the neck, and extensor surfaces of both distal arms and forearms of an 8-year-old girl. Erythema multiformetype lesions and distribution are similar to those of classic erythema multiforme, with lesions most frequent on the backs of the hands and extensor forearms. Pruriginous, erythematousedematous papules and plaques are located on both elbows. Systemic and discoid lupus erythematosus plaquelike lesions and histologic features may be identical to those 19 Light-Related Diseases and Disorders of Pigmentation 758. The characteristic direct and indirect immunofluorescence patterns of lupus erythematosus clarify the diagnosis. Treatment Topical steroids, antimalarial agents, and beta-carotene are often disappointing. In the case of minor complaints, patients can become disease free by using sunscreens and gradually increasing sun exposure in the spring. This rash is more common with the first sun exposure and lessens with repeated exposure. Short, intermittent 3- to 14-day courses of group I to V topical steroids are effective. Short courses of oral steroids are useful for very itchy, widespread eruptions or for patients who flare during a course of phototherapy or photochemotherapy. Doses small enough not to cause any abnormal reaction but large enough to 19 Light-Related Diseases and Disorders of Pigmentation 761 increase the tolerance of the skin to light are used. A regular series of such exposures, with small increments in exposure time, can result in an appreciable tolerance. Increments of 10% per exposure are given as long as there are no adverse reactions. A remission can be obtained for most patients by treatment two or three times each week for 4 to 12 weeks in the early spring. A number of patients remain protected for 2 to 3 months, even after pigmentation has faded. Maximum protection is reached 3 weeks after a 1 week course of treatment, and a single course offers a minimum of 6 weeks of protection. The course can be repeated each month during the spring and summer months if needed. Antimalarials need to be used only during the summer months; therefore the total necessary dose is small. A 3-month trial (hydroxychloroquine 400 mg/ day for the first month and 200 mg/day thereafter) has been effective in reducing rash and irritation. Although the risk of eye damage is slight, ophthalmologic examinations should be obtained periodically to monitor for antimalarial toxicity. Only 30% of patients responded satisfactorily to a dosage of 3 mg/kg body weight continued throughout the summer. The onset is before puberty (average age at onset is about 6 years), and males are affected more frequently than females. Avoidance of the sun and use of sunscreens, group V topical steroids, and wet compresses and antimalarials can control these diseases. A deficiency of any of the eight enzymes in the biosynthetic pathway can lead to a variety of clinical symptoms (Table 19. Each type of porphyria is associated with a specific enzymatic defect that results in an excess of a specific porphyrin (Tables 19. To control hydroa vacciniforme, patients should avoid the sun; apply sunscreens, topical steroids, and wet compresses. This childhood disease begins with the appearance of papules that progress to vesicles on sun-exposed skin of the cheeks. Lesions umbilicate, become necrotic, and heal with hypopigmented depressed (vacciniform or varioliform) scars. They are differentiated by measuring levels of heme precursors in urine, feces, erythrocytes, and plasma. Two main types of clinical manifestation occur: lifethreatening attacks of acute porphyria and skin photosensitization. All types show excess porphyrin metabolites in blood, urine, or feces and in various tissues such as skin and liver. Certain porphyrin metabolites (porphyrinogens) accumulate in the skin and are auto-oxidized to become porphyrins.
Lamotrigine dosages: 200 mg, 100 mg, 50 mg, 25 mgLamotrigine packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
Clinical manifestations and pathogenesis of cutaneous lymphomas: current status and future directions symptoms 1 week before period discount lamotrigine master card. Primary cutaneous B-cell lymphomas with large cell predominance-primary cutaneous follicle center lymphoma, diffuse large B-cell lymphoma, leg type and intravascular large B-cell lymphoma. The most common related cancers are rectal, genitourinary (including bladder, renal, and prostate), uterine, breast, hepatic, pancreatic, and adnexal. When an underlying malignancy is present, up to 50% of lesions have already metastasized. The risk of an associated internal malignancy is 14% in perianal disease and 20% in vulvar disease. Multicentric and vague margins may extend beyond the clinically detectable lesion. The course is unpredictable, ranging from indolent disease to aggressive malignancy. Lichen sclerosus et atrophicus, lichen simplex chronicus, leukoplakia, Bowen disease, or chronic yeast infections are in the differential diagnosis. Intraepithelial clusters of large round cells with oval vesicular nuclei and increased pale-staining cytoplasm are present. Histologically, Paget disease resembles Bowen disease and superficial spreading melanoma. Immunoperoxidase stains are helpful in establishing the diagnosis and in excluding conditions that resemble Paget disease. Tumor size does not predict nodal involvement; therefore, there is no primary tumor size that can reliably predict nodal involvement. Radiation of the regional lymph node basin and chemotherapy are therapeutic options. Three biopsies were taken before malignant cells were demonstrated at the periphery of this chronic ulcer at the base of the vulva. Cutaneous metastases may be the first sign of extranodal metastatic disease, particularly in patients with melanoma, breast cancer, or mucosal cancers of the head and neck. In a series of papers,22 Brownstein and Helwig stated several aspects of cutaneous metastasis. They determined the incidence and relative importance of the gender of the patient, the location of the metastatic growth, the morphology of the metastatic lesion, and the histologic features therapy, is the treatment for regionally confined disease. The tumor consists of small, round, blue cells similar in appearance to other small, round, blue cell tumors. The most helpful information for localizing the primary tumor is the gender of the patient and the location of the skin tumor. Accurate clinical diagnosis is rare; the lesions are most frequently diagnosed as cysts or benign fibrous tumors. In several instances, the clinical picture is that of a vascular tumor such as a pyogenic granuloma, hemangioma, or Kaposi sarcoma. The second most common pattern of cutaneous metastasis is inflammation with erythema, edema, warmth, and tenderness. The primary tumor is usually in the breast, and malignant cells spread to the subepidermal lymphatic vessels, where they create obstruction. The initial diagnosis is frequently a bacterial infection, such as erysipelas or cellulitis. The third and least common pattern simulates a cicatricial condition and resembles discoid lupus erythematosus or morphea. Carcinoma en cuirasse is seen with breast cancer and appears as a hard, infiltrated plaque with a leathery appearance that results from fibrosis and lymph stasis. In general, the histologic features of primary and metastatic tumors are similar, but metastatic tumors are often less differentiated. Frequently, biopsy specimens are not interpreted as originating from a distant site. Squamous cell carcinoma metastatic to the skin customarily originates from the oral cavity, lung, or esophagus. Tumors that invade veins, such as carcinoma of the kidney and lung, frequently present as cutaneous metastasis occurring in diverse skin sites distant from the primary tumor. Familial skin cancer syndromes: increased risk of nonmelanotic skin cancers and extracutaneous tumors. A randomized pilot comparative study of topical methyl aminolevulinate photodynamic therapy versus imiquimod 5% versus sequential application of both therapies in immunocompetent patients with actinic keratosis: clinical and histologic outcomes.
Satmooli (Asparagus Racemosus). Lamotrigine.
- Dosing considerations for Asparagus Racemosus.
- Pain, anxiety, stomach and uterine spasms, breast milk stimulation, uterine bleeding, premenstrual syndrome, alcohol withdrawal, indigestion, gastric ulcers, diarrhea, bronchitis, diabetes, dementia, and other conditions.
- What is Asparagus Racemosus?
- Are there safety concerns?
- How does Asparagus Racemosus work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=97111
Thrombocytopenia medicine bow lamotrigine 100 mg buy on-line, microangiopathic hemolytic anemia, and an acute or chronic consumption coagulopathy occur in association with a rapidly enlarging hemangioma. Consensusderived practice standards plan for complicated Kaposiform hemangioendothelioma. In most cases these distinctive lesions are developmental anomalies and are not due to a known gene mutation. They may be a few millimeters in diameter or may cover an entire limb and they grow in proportion to somatic growth. Two-thirds of all patients develop nodularity or hypertrophy by the fifth decade of life. Unlike the salmon patch, nevus flammeus tends to darken with age and may develop pyogenic granulomas. Ipsilateral glaucoma is frequent when nevus flammeus involves both the ophthalmologic and the maxillary divisions of the trigeminal nerve, but it is unlikely when the face is affected in either one of the upper divisions of the fifth cranial nerve or solely below the eye. The most common orodental manifestations are enlargement of the lips, stained gums, abnormal bite, and spontaneous bleeding of the gums. Hypertrophy is classified as thickened (25%), nodular (40%), or both thickened and nodular (35%). When it occurs over the midline of the back, nevus flammeus may be associated with an underlying spinal cord arteriovenous malformation. Variants exist where only one of these three structures is involved with the vascular malformation. These patients may develop seizures, headaches and migraines, stroke-like episodes, focal neurologic impairments, visual problems, and cognitive deficits. Lesions may become studded with papules and develop a cobblestone-like appearance. SturgeWeber syndrome (encephalotrigeminal angiomatosis) is a consideration in this patient. Centrofacial lesions and lesions involving maxillary areas in adults and children respond less favorably than lesions located elsewhere on the head and neck. Individuals are treated as outpatients; patients younger than 12 years of age usually require some form of sedation or anesthesia; the procedure is painful and cooperation during the procedure is necessary. The cosmetic appearance of some patients with nevus flammeus can be significantly improved by using the tinted waterproof makeup Covermark. These lesions fade within the first year of life, but may be seen during periods of crying. Nevus Simplex (Salmon Patch) Salmon patches are pink to red patches with indistinct borders found in 30% to 80% of newborns. The precise cause is unknown, but salmon patches are thought to be due to remnants of fetal circulation and fade in 1 to 3 years. Occiput and nape salmon patches have a tendency to be persistent and are found throughout life. Involvement of the entire V1 area puts the patient at high risk of having SturgeWeber syndrome. Some pregnant women show an increased number of cherry angiomas during pregnancy that involute in the postpartum period. The papules are easily removed by scissor excision or electrodesiccation and curettage and pulsed dye laser. Angiokeratomas Angiokeratomas are lesions characterized by dilation of the superficial dermal blood vessels and hyperkeratosis of the overlying epidermis. Increased venous pressure may be implicated, such as occurs with pregnancy and hemorrhoids. If desired, removal is performed by simple scissor excision or electrodesiccation and curettage. They consist of red-brown-black hyperkeratotic plaques varying in size and distribution. Numerous cutaneous angiokeratomas (angiokeratoma corporis diffusum) are part of Fabry Anderson disease (see Table 23.
Syndromes
- Impotence
- History of skin inflammation
- Genital herpes (small, painful blisters filled with clear or straw-colored fluid)
- Dizziness
- Impotence
- Blurred vision
- Being a health care worker
- Hypogonadism
In other patients medicine cabinet shelves lamotrigine 25 mg purchase online, the involved sites acquire broad areas of erythema, and the papules remain discrete. The mean duration is 6 weeks, but the rash is usually not severe for more than 1 week. Unlike urticaria, the eruption remains fixed and increases in intensity, clearing in most cases before or within 1 week after delivery. Pruritic urticarial papules and plaques of pregnancy are significantly associated with multiple pregnancies, hypertensive disorders, and induction of labor. Perinatal outcome is comparable to that of pregnancies without polymorphic eruption of pregnancy. There are no laboratory abnormalities, and direct immunofluorescence of lesional and perilesional skin is negative. The expectant mother can be assured that pruritus will quickly terminate before or after delivery. Itching can be relieved with group V topical steroids; cool, wet compresses; oatmeal baths; and antihistamines. Dermatological diseases associated with pregnancy: pemphigoid gestationis, polymorphic eruption of pregnancy, intrahepatic cholestasis of pregnancy, and atopic eruption of pregnancy. Atopic eruption of pregnancy includes eczematous and papular lesions in patients with an atopic background. Some patients have widespread eczematous changes affecting the face, neck, and flexural surfaces of the extremities. Others have just small erythematous papules disseminated on the trunk and limbs or prurigo nodules located on the shins and arms. Intrahepatic cholestasis of pregnancy is a reversible form of hormonally triggered cholestasis that develops in genetically predisposed woman in late pregnancy. A defect in the excretion of bile salts results in elevated levels of bile acids in the serum. Bile acids can pass into the fetal circulation and cause acute placental anoxia and cardiac depression. There is an increase of serum bile acid levels and liver function tests may be normal. Steatorrhea with malabsorption of fat-soluble vitamins including vitamin K (and potential bleeding complications) and cholelithiasis may occur. Pruritus stops after delivery but may recur with future pregnancies and oral contraception. In cases of jaundice and vitamin K deficiency, there is an increased risk for intra- and postpartum hemorrhage in both mother and child. A dosage of 15 mg/kg/day (typical dose 1 g/day) is taken as a single dose or divided into two to three doses until delivery. Urticarial vasculitis is a subset of vasculitis characterized clinically by urticarial skin lesions and histologically by necrotizing vasculitis. Immune complexes are thought to lodge in small blood vessels with activation of complement, degranulation of mast cells, infiltration by acute inflammatory cells, deposition of fibrin, and damage to blood vessels. Of affected patients, 32% have hypocomplementemia, 64% have lesions that persist more than 24 hours, 32% have painful or burning lesions, and 35% have lesions that resolve with purpura or hyperpigmentation. Extracutaneous features were present in 81%, hypocomplementemia in 11%, and abnormalities of other laboratory parameters. Patients with urticarial vasculitis have been categorized into two sub-groups: those with hypocomplementemia and those with normal complement levels. Normocomplementemic urticarial vasculitis is usually idiopathic, benign, and self-limited. This most common form has also been described in patients with monoclonal gammopathy, neoplasia, repeated cold exposure, and ultraviolet light sensitivity. Patients with hypocomplementemia are more likely to have systemic involvement than patients with normal complement levels.
Usage: a.c.
Combination regimens that include an antibiotic and a retinoid to reduce follicular plugging are the mainstay of topical treatment medications when pregnant 50 mg lamotrigine order. Pustular acne may respond quickly to drying therapy with a combination of benzoyl peroxide and sulfacetamide-sulfur lotion. Systemic therapy with antibiotics or isotretinoin is used when scarring occurs or for cystic acne. Topical agents should be applied to the entire affected area to treat existing lesions and to prevent the development of new ones. Potent topical steroid creams produce no short-term improvement in patients with moderate acne. Retinoids Retinoids reverse the abnormal pattern of keratinization seen in acne vulgaris. Agents that act in a comedolytic and anticomedogenic manner to reduce follicular plugging are the retinoids tretinoin, adapalene, and tazarotene, and isotretinoin. Retinoids initiate increased cell turnover in both normal follicles and comedones and reduce the cohesion between keratinized cells. They act Therapeutic Agents for Treatment of Acne There are four pathogenetic factors responsible for the development of acne. Animal studies have revealed no evidence of harm to the fetus; however, there are no adequate and well-controlled studies in pregnant women or Animal studies have shown an adverse effect, but adequate and well-controlled studies in pregnant women have failed to demonstrate a risk to the fetus. Animal studies have shown an adverse effect, and there are no adequate and well-controlled studies in pregnant women or No animal studies have been conducted, and there are no adequate and well-controlled studies in pregnant women. Adequate well-controlled or observational studies in pregnant women have demonstrated a risk to the fetus. Adequate well-controlled or observational studies in animals or pregnant women have demonstrated positive evidence of fetal abnormalities. The use of the product is contraindicated in women who are or may become pregnant. Continual topical application leads to thinning of the stratum corneum, making the skin more susceptible to sunburn, sun damage, and irritation from wind, cold, or dryness. Irritants such as astringents, alcohol, and acne soaps will not be tolerated as they were previously. Topical erythromycin in combination with benzoyl peroxide (5% maximum) can be used as alternative treatment for inflammatory acne. Topical clindamycin in combination with benzoyl peroxide can be used as alternative treatment for inflammatory acne. Topical dapsone is a newer anti-acne agent with less available safety data and should be used with caution in pregnant patients. Intralesional steroid injections can be used to treat moderate to severe inflammatory acne. Oral glucocorticoids can be used short term to treat fulminant acne after the first trimester. Retinoids enhance the penetration of other topical agents such as topical antibiotics and benzoyl peroxide. The enhanced penetration results in a synergistic effect with greater overall drug efficacy and a faster response to treatment. The relative benefit of adapalenebenzoyl peroxide increases with higher lesion counts at baseline. To minimize possible irritation, the skin should be allowed to dry completely by waiting 20 to 30 minutes before application of retinoids. Patients with sensitive skin or those living in cold, dry climates may start with an application every other or every third day. The frequency of application can be gradually increased to as often as twice each day if tolerated. The corners of the nose, the mouth, and the eyes should be avoided; these areas are the most sensitive and the most easily irritated. Retinoids are applied to the chin less frequently during the initial stages of therapy; the chin is sensitive and is usually the first area to become red and scaly. One to four weeks: During the first few weeks, patients may experience redness, burning, or peeling. Those tolerating daily applications may be advanced to a higher dosage or to the more potent solution. Three to six weeks: New papules and pustules may appear because comedones become irritated during the process of being dislodged.
References
- Cassileth BR, Upkis RV, Sutton-Smith K, et al: Informed consent-why are its goals imperfectly realized?, N Engl J Med 302(16):896-900, 1980.
- Mabillard H, Srivastava S, Haslam P, et al: Large retroperitoneal haemorrhage following cyst rupture in a patient with autosomal dominant polycystic kidney disease, Case Rep Nephrol 2017:2017.
- Shepherd JH, Sideri M, Maisonneuve P, et al. Carcinoma of the vagina. FIGO Annual Report on the results of the treatment in gynaecological cancer. J Epidem Biostat. 1998;3:1.
- Risau W: Mechanisms of angiogenesis, Nature 386(6626):671-674, 1997.
- Maki KC, Dicklin MR, Davidson MH, et al. Baseline lipoprotein lipids and low-density lipoprotein cholesterol response to prescription omega-3 acid ethyl ester added to simvastatin therapy. Am J Cardiol 2010;105:1409-1412.
- Leppilahti, M., Sairanen, J., Tammela, T.L., Aaltomaa, S., Lehtoranta, K., Auvinen, A. Prevalence of clinically confirmed interstitial cystitis in women: a population based study in Finland. J Urol 2005;174:581-583.