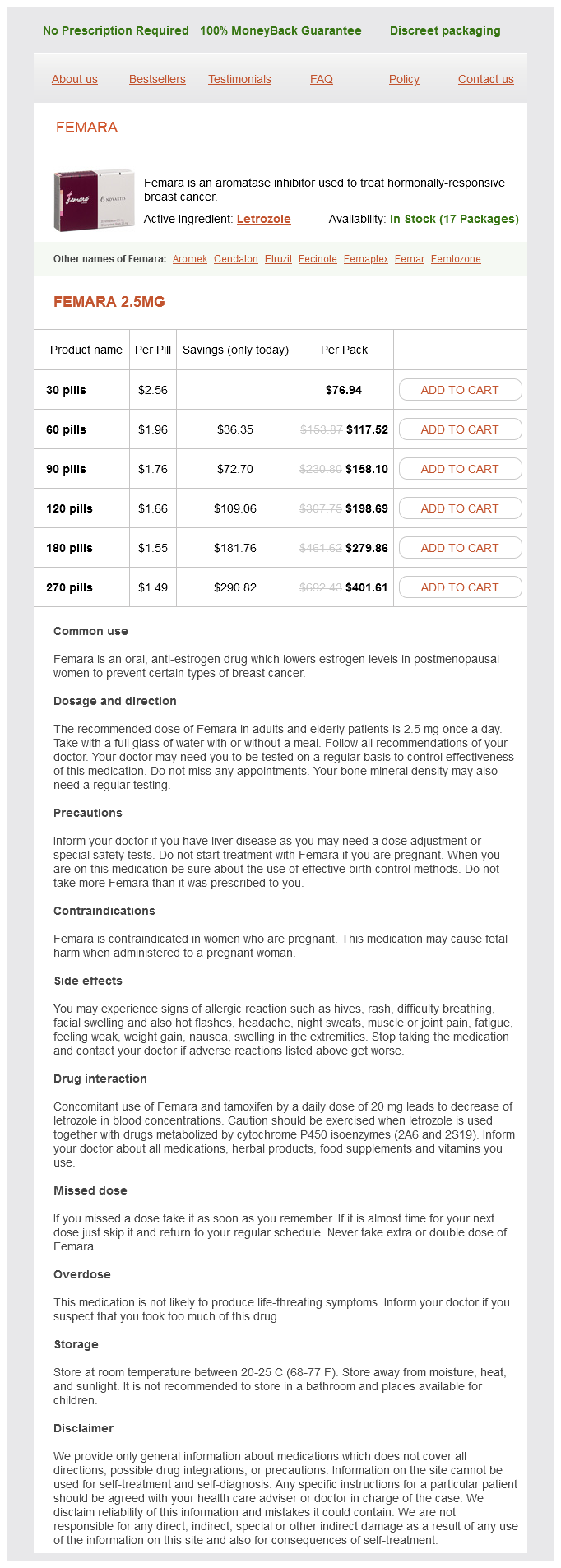
Femara
Femara 2.5mg
- 30 pills - $76.94
- 60 pills - $117.52
- 90 pills - $158.10
- 120 pills - $198.69
- 180 pills - $279.86
- 270 pills - $401.61
As such pregnancy outfits order femara visa, it is an increasingly useful tool in the diagnosis of specific cardiomyopathies. Major limitations are incompatibility with most implanted electronic cardiovascular devices and the potential for nephrogenic sclerosing fibrosis with the use of gadolinium-based contrast agents in patients with preexisting renal insufficiency (see Chapter 51). Invasive hemodynamic monitoring is often helpful in the diagnosis and inpatient management of heart failure. Right heart catheterization can be combined with exercise testing or infusions of inotropic or vasodilatory agents to study their hemodynamic effects. Reasonable indications for right heart catheterization include short-term management of acute cardiogenic shock, evaluation of patients for cardiac transplantation or mechanical circulatory support, clarification of hemodynamics in the context-specific comorbidities. Cardiac output/index is one of the important measurements provided by right heart catheterization. Right atrial pressure is an important indicator of volume status and right heart function. An elevated central venous pressure has been shown to be the most important predictor of worsening renal function during hospitalizations for acute decompensated heart failure. There are many approaches to determining which patients with systolic heart failure warrant evaluation by coronary angiography. The Heart Failure Society of America recommends performing coronary angiography in patients with a high pretest probability of underlying ischemic cardiomyopathy and who are candidates for percutaneous or surgical revascularization. Some centers advocate for a baseline coronary angiogram in all patients with newly established systolic heart failure regardless of risk factors or presentation. Endomyocardial biopsy (see Chapter 61) is indicated only when a specific primary myocardial disease is suspected and other causes of decompensation have been ruled out. Cardiopulmonary exercise testing (metabolic stress testing) while not recommended as part of the routine evaluation of patients with heart failure should be considered in the context of symptoms out of proportion with objective measures of disease severity, discriminating between cardiac and pulmonary etiologies of dyspnea, or assessing candidacy for cardiac transplantation or mechanical circulatory support. Several routinely measured parameters are highly predictive of prognosis in patients with established heart failure. Peak oxygen consumption (Vo2) is perhaps the most important parameter in objectively describing functional capacity and prognosticating. Normal values based on age and sex are indexed to body weight, with a normal value being > 84% predicted. Patients with a peak Vo2 < 14 mL/ kg/min or < 50% predicted are at increased risk for adverse cardiovascular events and if the limitation is deemed to be cardiac should be considered for transplantation. It signifies the conversion to anaerobic metabolism and the sudden rise in co2 production occurring with the onset of metabolic acidosis. Ventilatory anaerobic threshold is another means of assessing the adequacy of effort and represents the point at which minute ventilation (Ve) increases out of proportion with Vo2 (typically occurring at 60% to 70% of peak Vo2). The slope is elevated in most patients with heart failure and is inversely related to cardiac output at peak exercise. Obstructive sleep apnea and central sleep apnea are common comorbidities contributing adversely to the pathogenesis and prognosis of patients with heart failure. The effective management of heart failure relies on appreciating the distinction between acute and chronic therapies. The initial management goals include symptom improvement, decongestion, and hemodynamic stabilization with optimization of tissue perfusion. It is important to attempt to identify and correct any precipitating factors (Table 8. The use of a pulmonary artery catheter should therefore be restricted to the scenarios detailed above where there is need for clarification of cardiac indices or filling pressures and in critically ill patients failing to respond to standard therapies. Continuous blood pressure monitoring with an arterial catheter can be useful in cases with marginal blood pressure and allows for optimal titration of intravenous vasodilators. In the absence of symptomatic hypotension, intravenous vasodilators are the first-line therapy for the management of cardiogenic pulmonary edema. While there is no maximal dose, increasing beyond 300 to 400 g/min likely yields no additional benefit and should prompt the addition of another vasodilator. Sodium nitroprusside is a potent vasodilator with balanced venous and arteriolar effects. Nitroprusside is particularly useful in instances where a rapid and large reduction in afterload is desired. While cyanide and thiocyanate toxicity is exceedingly rare with short durations of therapy, nitroprusside should be used with caution in patients with severe renal dysfunction.
Femara dosages: 2.5 mgFemara packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills
The assessment of noncancer risk by air toxics to any organ system is based on the computation of long-term risk reference exposure concentrations (RfCs) to which individuals may be exposed over a lifetime without adverse menopause vs pregnancy symptoms discount 2.5 mg femara, irreversible injury. An analogous short-term RfC method has been developed for exposures up to 30 days. Of the noncancer risks deemed itself to use as a model pulmonary toxicant for studies addressing C × T relationships. These studies suggest that there may be a threshold below which compensatory and other bodily defenses (eg, antioxidants) may be able to cope with long-term low-level exposure (tolerance). For phosgene, this appears to be at or below the current threshold limit value of 0. At higher concentrations, however, concentration appears to be the primary determinant of injury or disease regardless of duration. Thus, even though there is some adaptation with time, there continues to be a concentration-driven response that exceeds that predicted by C × T. This relationship appears to be different from that of O3 at ambient levels, which can be approximated acutely by the C × T paradigm. The breadth and complexity of the problem of air pollution-from the development of credible databases to supporting regulatory action and decision making-has been the theme throughout. The classic and still most important air pollutants provide a foundation for understanding and appreciating the nuances of the issues and strategies for air pollution control and protection of public health. The key role of the toxicologist is to develop sensitive methods to assay responses to low pollutant concentrations, apply these methods to relevant exposure scenarios and test species, and develop paradigms to relate empirical toxicological data to real life through an understanding of mechanism. Last, the toxicologist must continually integrate laboratory data with those of epidemiology and clinical study to ensure their maximum utility. These complexities have been daunting to toxicologists for decades and have prompted scientists and risk assessors to adopt a reductionist approach-nominally one pollutant at a time. While the reductionist approach has been very successful in diminishing pollutants of primary concern and improving public health, it is widely thought that there are likely chemical and physiologic interactions between and among pollutants that are of public health consequence and have not been appreciated. As the science and the statistical methods to look at interactions have improved, there is renewed interest in multipollutant toxicology. There is yet to be any consensus on any of these aspects of multipollutant science other than this is the appropriate time to reinitiate the discussion. Early toxicology studies used complex mixtures, some of which were photochemically altered (discussed earlier), and epidemiology found that different mixtures appeared to vary in their health impacts, only to abandon the task. While single pollutant approaches to air pollution research, health assessments, and ambient air quality standard setting have been successful in reducing air pollution over the past few decades, there is a clear need for parallel efforts within both the scientific and the regulatory/policy communities to advance methods for evaluating and managing the effects of air pollution in a multipollutant manner. Sensory and pulmonary irritation of methyl isocyanate in mice and pulmonary irritation and possible cyanidelike effects of methyl isocyanate in guinea pigs. Short-term effects of carbon monoxide exposure on individuals with coronary heart disease. The response of guinea pigs to inhalation of formaldehyde and formic acid alone and with a sodium chloride aerosol. An estimate of the global burden of anthropogenic ozone and fine particulate matter on premature human mortality using atmospheric modeling. Air pollution and hospital admissions in southern Ontario: the acid summer haze effect. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Histopathological changes of the nasal mucosa in southwest metropolitan Mexico City inhabitants. Epithelial injury and interstitial fibrosis in the proximal alveolar regions of rats chronically exposed to a simulated pattern of urban ambient ozone. Alveolar epithelial cell injuries by subacute exposure to low concentrations of ozone correlate with cumulative exposure. Atherosclerosis lesion progression during inhalation exposure to environmental tobacco smoke: a comparison to concentrated ambient air fine particles exposure. Acute toxicity of irradiated auto exhaust: its indication by enhancement of mortality from streptococcal pneumonia. Human respiratory tract cancer risks of inhaled formaldehyde: doseresponse predictions derived from biologically-motivated computational modeling of a combined rodent and human dataset.
Carboxyethylgermanium Sesquioxide (Germanium). Femara.
- Dosing considerations for Germanium.
- Are there any interactions with medications?
- Arthritis, pain relief, osteoporosis (weak bones), low energy, AIDS, cancer, high blood pressure, high cholesterol, heart disease, glaucoma, cataracts, depression, liver problems, food allergies, yeast infections, ongoing viral infections, heavy metal poisoning, increasing circulation of blood to the brain, supporting the immune system, use as an antioxidant, or other uses.
- Are there safety concerns?
- How does Germanium work?
- What is Germanium?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96468
Women typically have a skin-sparing mastectomy with removal of the nipple-areolar complex menopause relief products purchase femara 2.5 mg fast delivery. On imaging, fatty tissue replaces the breast mound with scars in the subcutaneous regions. Most local recurrence will occur between years 1 and 7 after lumpectomy, with the peak at year 4. Right mammogram shows a small mass between the lumpectomy bed and the nipple (arrow). Four years after lumpectomy, the scar is increasing in density (arrow) compared with 2 years prior. Local Occurrence in a Tissue Flap Local recurrence in a tissue flap occurs in the residual breast tissue, not the relocated abdominal fat. Because many women now have skin-sparing mastectomy, local recurrence typically occurs along the subcutaneous scar line. T1 postcontrast images show nonmass enhancement at the lumpectomy scar (blue arrow), linear nonmass enhancement anterior to the scar (yellow arrow), and a round enhancing mass lateral to the scar (green arrow). Some areas in the right breast have regressed, although other focal areas have become more prominent. Note that the mass is just superficial to the scar from the skin-sparing mastectomy (arrow). Distortion and density of a postsurgical scar are most pronounced on the first postoperative study, whether due to benign biopsy or lumpectomy for cancer. View small masses or calcifications in the same ductal system as the original cancer (between the scar and the nipple and the scar and the chest wall) with suspicion. The key to detecting recurrent breast cancer on mammography is change over time based on comparison with previous mammograms. After stabilization of the post-therapeutic changes, any new or more prominent findings should be viewed with suspicion. Mammographic findings of recurrent breast cancer after lumpectomy and radiation therapy: Comparison with the primary tumor. The efficacy of specimen radiography in evaluating the surgical margins of impalpable breast carcinoma. Detecting residual tumor after excisional biopsy of impalpable breast carcinoma: Efficacy of comparing preoperative mammograms with radiographs of the biopsy specimen. How do you explain the enhancement in the posterior aspect of the reconstructed breast (arrow) There are bilateral inferior scars with a distribution typical for reduction mammoplasty. The scars in the inferior breast and areolar region are identified by the signal dropout artifact from metallic fragments that occur during the surgical procedure, often associated with use of the electrocautery device. Did you notice that the mass contains fat on the T1 precontrast image without fat saturation She had reduction mammoplasty on the left at the time of her mastectomy for symmetry. There is increasing density at the lumpectomy site that is inconsistent with the normal evolution of post-treatment changes. Although echogenic lesions are usually benign, the change on mammography is suspicious and warrants biopsy. There are multiple rim-enhancing masses in the posterior right breast with high signal on T1 indicative of fat. It would be prudent for the surgeon to remove a little more tissue at the deep end of the surgical bed (where the tip of the wire is located). The pathologist did find a positive margin on the original lumpectomy sample, but the margins of the additional tissue taken by the surgeon were negative. Her lumpectomy scar is located in a different quadrant (yellow arrow), so this is more likely to be a second primary carcinoma rather than local recurrence. There is increased signal intensity with signal dropout at the edges located at the lumpectomy site on the T1 postcontrast sequence (arrow). This could be due to signal flare from a clip in the lumpectomy bed or local recurrence.
Syndromes
- Enlargement of the colon (megacolon)
- Tuberculosis
- Hypophosphatemia
- MPS I H (Hurler syndrome)
- Dumping syndrome
- Glaucoma
- Name of the product (ingredients and strengths, if known)
- Do you have eye pain or other symptoms, including headache, stuffy or runny nose, or joint or muscle aches?
However menstruation bible discount femara on line, aminoglycoside resistance represents the most common and grave obstacle to optimal therapy for enterococcal endocarditis. However, staphylococci have a relatively high intrinsic mutation rate for the gene controlling the site of rifampin action. Therefore, when large populations of staphylococci are exposed to rifampin, selection of rifampin-resistant organisms is common. Often, antistaphylococcal agent(s) may be administered for 3 to 5 days to reduce the total number of staphylococci before the commencement of rifampin. A multidrug approach (two antibiotics that are known to be active against the staphylococcal isolate in addition to rifampin) may reduce the probability of developing rifampin-resistant subpopulations. Renal function is an important consideration when using aminoglycosides or vancomycin. In fact, simultaneous treatment with penicillin and heparin increases the risk of fatal intracerebral hemorrhage. Empiric therapy should cover the most likely pathogens, including staphylococci (both methicillin-sensitive and methicillin-resistant strains), streptococci, and enterococci. Afluoroquinolone should be considered as an alternative agent for patients unable to tolerate -lactam therapy. The final choice of antibiotic therapy is to be made after sensitivity results are available. After 1 to 2 weeks of full-dose amphotericin B therapy, surgery should be performed because effective penetration of the medicine into vegetations is unlikely. Long-term oral suppressive therapy with antifungal agents such as fluconazole or itraconazole is commonly recommended to prevent relapse. Surgery is indicated in approximately 25% to 30% of cases during the acute phase of infection and in another 20% to 40% in subsequent or secondary phases. Controversial indications include the presence of more than one serious systemic embolic event or one embolus with a large residual vegetation. The best management in the scenario of hemodynamic instability and new-onset embolic stroke has not been addressed in randomized clinical studies. However, some patients may need early surgery despite a recent stroke if they are at high risk for recurrent emboli. If a mycotic aneurysm is found, the timing of surgery should be reconsidered, and any prosthesis that requires postoperative anticoagulation should be avoided. A ruptured mycotic aneurysm should be resected, clipped, or embolized before cardiac operation. For patients with positive intraoperative cultures, a full course of therapy should be given postoperatively. The success rate without removal of the entire device is low because typically the entire device is infected. Most studies suggest that the complete explantation of all hardware combined with antibiotic therapy is the optimal management. Studies have shown that reimplantation is successfully performed at a median of 7 days (5 to 25 days) after explantation. Significant enlargement of a vegetation during treatment indicates possible treatment failure and constitutes a relative indication for surgery. Generally, if fever persists for more than 7 days or if blood cultures are positive beyond the first week of antibiotic therapy, the treatment is considered a failure. Relapses, should they occur, usually manifest clinically within 4 weeks and can be confirmed by blood cultures. The frequency of emboli falls rapidly after 1 to 2 weeks of antibiotic therapy, and the risk is considered to be greatest in the setting of large vegetations (> 10 mm in diameter) and specific infections (S. One barrier to the development of this model is inconsistencies in the prognostic value of individual parameters in the published data. These differences may in part be due to time dependencies of various risk factors. A recent study used the Society of Thoracic Surgery database to develop a surgical mortality risk scoring system. Although several studies have attempted to evaluate the most significant predictors of risk, a standardized risk scoring model has yet to be established. Endocarditis prophylaxis following dental or oral procedures is directed primarily against viridans Streptococcus; following genitourinary and gastrointestinal surgery it is directed primarily against Enterococcus organisms. For nonoral soft-tissue infections, an antistaphylococcal penicillin or first-generation cephalosporin is an appropriate choice of prophylaxis.
Usage: q._h.
Troponins C ardiac troponins are proteins that regulate the calcium-dependent interactions between actin and myosin women's health center naperville il femara 2.5 mg purchase with amex. Troponin this a myofibrillary protein and is a constituent of the contractile apparatus of cardiac muscle. A quantitative relation has also been demonstrated between levels of cardiac troponin T and long-term clinical outcome. Qualitative and quantitative point-of-care tests for troponin T and troponin I are fast, yielding results that are reliable and accurate within a few minutes. Plasma myeloperoxidase levels are elevated in persons with angiographically documented coronary disease and within culprit lesions prone to plaque rupture. Investigations aimed at overcoming these problems have focused on myocardial perfusion and functional imaging. Two-dimensional echocardiography provides valuable diagnostic data on ventricular function and regional wall motion abnormalities. Myocardial ischemia can cause abnormal segmental function of the myocardium manifested as impaired relaxation, hypokinesis, akinesis, or dyskinesia. Normal findings at echocardiography cannot be used reliably to rule out myocardial ischemia. Areas of myocardium with a negative scintigraphic image, indicating decreased myocardial uptake, can be demonstrated in ischemic or infarcted myocardium within 6 hours of symptom onset. The diagnostic utility of such imaging is limited by the so-called moment-in-time problem; perfusion defects may represent acutely ischemic myocardium or preexisting areas of scar tissue. Thallium 201 imaging has relatively poor specificity in women because of difficulties in distinguishing between breast attenuation and perfusion defects caused by coronary artery disease. Technetium 99m sestamibi tomographic imaging has the advantage that it does not redistribute after initial injection. This type of imaging allows definition of an initial ischemic zone that can be studied even after reperfusion. Technetium-derived image quality is also superior to that of thallium and allows quantification of regional and global ventricular function by gated image acquisition. Perfusion imaging with technetium 99m appears to have a sensitivity equivalent to that of thallium 201 imaging in defining myocardium at risk. The main limitation of this technology lies in the inability to determine the physiologic significance of coronary lesions of intermediate severity. Differentiating ischemic from nonischemic causes of chest pain can be difficult (Table 36. Given that there is symptom overlap among a number of clinical entities, in most diagnostic strategies, it is assumed that chest pain is cardiac in origin until proven otherwise. It is important to understand the clinical characteristics that represent the leading noncardiac causes of chest pain. Pericarditis (see Chapter 40) is often accompanied by substernal chest pain, but the pain is more likely to be pleuritic in character and aggravated by recumbency, deep inspiration, and swallowing. In addition, the presence of pulsus paradoxus, defined as an abnormally large (> 10 mm Hg) decline in systolic blood pressure during inhalation, is a very helpful sign in cardiac tamponade and reflects exaggerated ventricular interdependence, the key pathophysiologic mechanism in this life-threatening condition. Prompt bedside echocardiography wherever possible is very useful in confirmation of the diagnosis as well as guidance for percutaneous pericardiocentesis. Aortic dissection (see Chapter 26) requires urgent diagnosis because early surgical intervention reduces the high short-term mortality rate. The chest pain of aortic dissection is typically described as sudden, severe, and tearing pain that radiates to the back and interscapular areas, which is most intense at onset. Examination may reveal a difference in right and left arm blood pressures, pulse deficits, and focal neurologic deficits. All these imaging modalities have high sensitivity and specificity in the diagnosis of acute aortic dissection. Pulmonary embolism is potentially life threatening and can be associated with chest pain. There is often a history of recent surgical intervention, malignant disease, or immobility. However, when imaging results are inconsistent with clinical suspicion, additional testing in the form of V/Q scan or lower extremity ultrasonography may be necessary. Many patients will present with noncardiac conditions for chest pain, some of which are life threatening. The highest risk patients require emergent reperfusion therapy, whereas lower risk patients can undergo urgent invasive therapy or further risk stratification.
References
- Danhauser K, Sauer SW, Haack TB, et al. DHTKD1 mutations cause 2-aminoadipic and 2-oxoadipic aciduria. Am J Hum Genet 2012;91:1082.
- Ruts L, Drenthen J, Jacobs BC, van Doom PA. Distinguishing acute-onset CIDP from fluctuating Guillain-Barre syndrome: A prospective study. Neurology. 2010;74:1680-1686.
- Zipes DP, DiMarco JP, Gillette PC, et al. Guidelines for clinical intracardiac electrophysiological and catheter ablation procedures: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Clinical Intracardiac Electrophysiologic and Catheter Ablation Procedures), developed in collaboration with the North American Society of Pacing and Electrophysiology. J Am Coll Cardiol. 1995;26:555-573.
- Tu K, Mamdani MM, Hux JE, Tu Jun-bi. Progressive trends in the prevalence of benzodiazepine prescribing in older people in Ontario, Canada. J Am Geriatr Soc 2001;49:1341-5.
- ACC/AHA guidelines for the management of patients with valvular heart disease. A report of the American College of Cardiology/American Heart Association. Task Force on Practice Guidelines (Committee on Management of Patients with Valvular Heart Disease), J Am Coll Cardiol 32:1486, 1998.