Cialis Jelly
Cialis Jelly 20mg
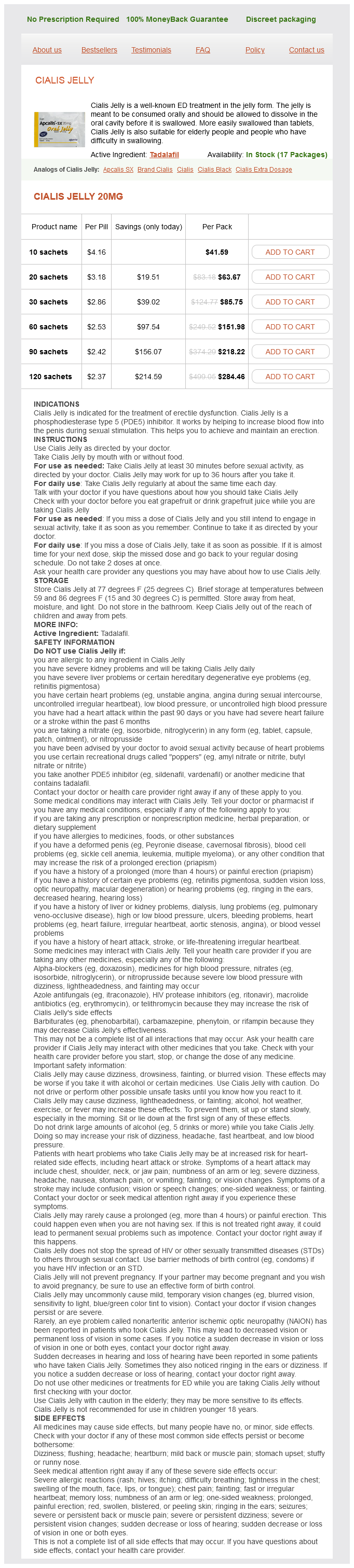
- 10 sachets - $41.59
- 20 sachets - $63.67
- 30 sachets - $85.75
- 60 sachets - $151.98
- 90 sachets - $218.22
- 120 sachets - $284.46
This step in screw placement is important because recession of the screw head into the bone prevents the patient from feeling a prominent screw head when he or she sits against a hard-backed chair erectile dysfunction doctor in houston cialis jelly 20 mg order overnight delivery. It is important to note that some prominence of the pelvic screw heads may be unavoidable in thin patients who have limited muscular covering of the lumbosacropelvic area. However, burying the screw heads below the superficial portion of the posterior superior iliac spine helps to prevent superficial skin breakdown and pressure sores in these patients. It is important to create the pelvic screw connection to the lumbosacral rod inferior to S1 to avoid interference of rod linkage with the S1 screw (if present). In the past we have used iliac bolts (fixed angle iliac screws) to fixate the pelvis and connect them with closed connectors to the lumbosacral rod. Thus the patient underwent a long segment correction and fusion of her kyphoscoliosis. Given the large flexion forces that would result from the length of this construct, the decision was made to extend the instrumentation to the pelvis. The patient underwent T3-S1 pedicle screws with bilateral pelvic screws followed by L4-5 and L5-S1 anterior interbody fusion. High-Grade Spondylolisthesis or Pseudoarthrosis Following Fixation for L5-S1 Spondylolisthesis Fusion rates in high-grade spondylolisthesis patients at the L5-S1 level are lower than fusion rates for degenerative spondylosis in the lumbar spine. Long Segment Fusion for Scoliosis Traditionally, long segment fusions in patients with idiopathic scoliosis with extension to the sacrum have resulted in high rates of pseudarthrosis at the S1 level. Extension of the construct to the pelvis with iliac screws decreases the strain on the sacral pedicle screws. The patient then presented to us with worsening bilateral lower extremity symptoms with radiographic progression of listhesis. High flexion forces are present at the sacrum in cases of high-grade spondylolisthesis; hence, the operative management strategy for this patient included pedicle screw fixation from L3 to S1 with extension to the pelvis. Sacral Osteolytic Neoplasms and Osteomyelitis Osteolytic destruction of the lumbar and sacral bony elements in patients with a neoplastic or infectious process presents a unique challenge for stabilization of the lumbosacral spine. When a neoplastic or infectious process has eroded the pedicle fixation points at S1, stabilization must be considered beyond the sacrum. Gokaslan and others have reported their experience in the stabilization of similar scenarios, primarily using a modified Galveston L-rod technique. Often, the purpose of iliac screws is to stress-shield S1 pedicle screws until fusion has occurred across the lumbosacral junction. Only in cases where S1 screw fixation is not possible (due to tumor or infection) do we make an attempt to fuse from the lumbar spine onto the medial ilium (which requires a significant volume of bone graft). The absence of fixation points at L5 and S1 prompted the use of instruments in the ala and ilium after débridement of the phlegmon. Complications As with any instrumented fusion, hardware failure, pseudarthrosis, and screw pull-out are observed complications when instrumenting the sacropelvis. The risk of pseudarthrosis at S1 may be minimized by aiming the S1 screws at the sacral promontory to achieve anterior cortical fixation. In addition, anterior column augmentation with interbody cage support is also helpful to minimize pseudarthrosis. Given the number of vascular, neural, and enteric structures contained within the sacropelvic bowl, misplaced iliac screws may have substantial morbidity. For instance, errant iliac screws could potentially injure structures within the greater sciatic notch or violate the acetabulum. Nevertheless, vascular or neural injuries have not been reported among the large series of pelvic screw fixations in the literature. The immediate perioperative complications are related to the extensive surgical exposure that may be required for this technique. For example, risk of infection (approximately 4%) and high volumes of blood loss have been reported with long segment spinal fixation extending to the pelvis. Midterm complications have been related to prominence of the hardware, which can be avoided by recessing the screw heads into the iliac spine, ensuring adequate soft tissue coverage. Moreover, iliac fixation allows for caudal fixation in cases where the sacrum is destroyed by neoplasms or osteomyelitis. Although sacropelvic fixation is not indicated as part of routine lumbosacral fusions, it enhances the rigidity of long segment fusions (L2-S1 or longer constructs) for correction of scoliosis and further stabilizes the lumbosacral junction in pseudarthrosis and high-grade spondylolisthesis cases. The Galveston experience with L-rod instrumentation for adolescent idiopathic scoliosis.
Cialis Jelly dosages: 20 mgCialis Jelly packs: 10 sachets, 20 sachets, 30 sachets, 60 sachets, 90 sachets, 120 sachets
Calcitonin is secreted by thyroid parafollicular cells and increases calcium stores in bone by inhibiting osteoclast activity impotence is a horrifying thing purchase genuine cialis jelly on line. Adequate nutrition with an appropriate balance of calcium and vitamin D is essential for optimizing bone quality. Calcium supplementation in the form of calcium carbonate or calcium citrate is primarily effective for postmenopausal women. With impact loading, differences in electronegative potential occur across compressed surfaces, which subsequently stimulates bone formation. An active exercise program of jogging and stair climbing in postmenopausal women receiving calcium supplementation resulted in a 5. Prolonged bed rest, however, can increase loss of bone density, result in muscle atrophy, and impair the functional outcome. Use of narcotics to alleviate pain can alter mood and cognitive function, which may further compound any existing medical and age-related conditions. Alternatively, surgical intervention consisting of spinal reconstruction and instrumented stabilization is limited in this population because of poor bone stock and generally high surgical risk stratification. The primary function of vertebroplasty and kyphoplasty is to decrease pain and improve mobility and function. Contraindications to these procedures include fractures with disruption of the posterior vertebral wall, neurological deficit, or complete collapse of the vertebral body. A Jamshidi needle is inserted percutaneously under biplanar fluoroscopic guidance via either a transpedicular or extrapedicular route into the affected level. Contrast medium is then injected through the needle to ensure that the tip is not within a vessel. The volume of injection is limited by the potential for extravertebral extravasation of cement. Kyphoplasty is similar to vertebroplasty in that a cannula is introduced percutaneously into the fractured vertebral body under fluoroscopic guidance. An inflatable bone tamp is then placed through the cannula and, on inflation, reduces the fractured fragments, thereby creating a cavity and restoring vertebral body height. This process may cause thermal necrosis of pain receptors within bone and a resultant decrease in sensitivity. Clinical studies of both vertebroplasty and kyphoplasty demonstrate significant beneficial results. The risk for extravasation of cement after vertebroplasty is widely variable and estimated to be 30% to 67%. Kyphoplasty is primarily differentiated from vertebroplasty in its potential for restoring vertebral body height and improving overall sagittal alignment. The average restoration of vertebral height with kyphoplasty is reported to be 30% to 35%. In a retrospective study of 65 patients undergoing one- to three-level kyphoplasty, Pradhan and colleagues found that kyphoplasty improved the local deformity at the fracture level by an average of 7. At three levels above and below the fracture level, the correction decreased to just 1. The researchers surmised that the majority of the local angular and height correction becomes negated at more distant levels by the relatively softer intervertebral disks. As a result, the radiographic improvement in overall sagittal alignment with kyphoplasty is modest at best. A metaanalysis of the literature revealed that both kyphoplasty and vertebroplasty result in a significant improvement in visual analog pain scores, with an average decrease of 5. The significant difference in risk for leakage of cement is hypothesized to be due to the injection of higher viscosity cement into the preformed cavity with kyphoplasty. Spine surgery in this population frequently involves instrumented stabilization and reconstruction. However, the use of rigid spinal fixation in the setting of osteoporosis can pose significant technical challenges. As bone quality weakens, the risk of loosening at the implant-bone interface increases under cyclic mechanical loading. Hardware failure in osteoporotic patients may also occur when increased biomechanical demands are placed on the instrumentation, such as when performing spinal corrective maneuvers. Ultimately, screw pullout may lead to loss of correction or progression of deformity. Longsegment rigid constructs also alter the biomechanical environment of the segments adjacent to the instrumentation.
Cordyceps. Cialis Jelly.
- Improving athletic performance.
- Are there safety concerns?
- How does Cordyceps work?
- Dosing considerations for Cordyceps.
- Are there any interactions with medications?
- Promoting longevity, decreasing fatigue, cough, bronchitis, breathing disorders, kidney disorders, male sexual dysfunction, anemia, heart arrhythmias, high cholesterol, liver disorders, kidney disorders, dizziness, weakness, ringing in the ears, improving quality of life after cancer chemotherapy, improving immune system function after cancer chemotherapy, improving liver function in people with hepatitis B, and other conditions.
- What is Cordyceps?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96597
Gentle traction may be applied with the retractor on the thecal sac if the level of the osteotomy is below the conus erectile dysfunction pump hcpc purchase cialis jelly without prescription. After circumscribing the pedicle, decancellation is performed through the residual pedicle stump. The residual pedicle stump is removed with a Leksell rongeur, and both sides are now made flush with the level of the vertebral body. The extent of decancellation depends on the amount of bone to be removed as determined during preoperative planning. Straight and curved curets are then used to perform decancellation through the pedicles and extended in wedge fashion into the vertebral body with the apex at the anterior cortex. Use of the curet should be controlled and meticulous with close attention paid to the surrounding neural structures. Bleeding during the decancellation procedure is managed with the intermittent use of hemostatic agents and tamponade with cottonoids. The cancellous bone behind the posterior vertebral cor- tical wall is removed thoroughly to make the wall as thin as possible. This cancellous bone should be saved for the future posterolateral fusion portion of the procedure. The final step in completing the osteotomy involves developing the epidural space between the posterior cortex and anterior dura with a Woodson elevator. Epidural bleeding is addressed by careful bipolar cauterization and judicious use of hemostatic agents. The posterior cortex is pushed down with the reversed-angle curet into the potential space created by the decancellation procedure to produce a greenstick fracture. Symmetrical removal of the posterior cortical wall is performed along with meticulous removal of all residual bone fragments or spicules. Before closure of the osteotomy, a Kerrison rongeur is used to further enlarge the central canal and remove any bone fragments that may interfere with the exiting nerve roots. The opposing bone surfaces are also made symmetrical with a Leksell or Kerrison rongeur. On one side, an appropriately sized rod is contoured and fixed to the screws loosely with caps. The compressor is placed along the head of the pedicle screws on each side and gently compressed to close the osteotomy defect. While maintaining compressive force, the caps are tightened and the rod is secured to the screw. Multiple sequential compression steps may be required for complete bone apposition. If the osteotomy is not completely closed, one should check for intervening residual bone fragments, inadequate rod contouring, or subluxation of the proximal elements. In situ benders may be used to recontour the rod and compressive forces then reapplied. The proximal spinal elements may sublux dorsally with respect to the distal elements. Such subluxation needs to be reduced to achieve anatomic alignment before final tightening of the implant. Finally, a Woodson elevator is used to facilitate inspection of the thecal sac and the nerve roots to make certain that there is no bone compression or any compromise of the neural structures. The procedure is completed by posterolateral decortication with a drill and placement of the bone graft harvested from the osteotomy procedure. A subfascial drain is placed and the wound is closed in standard multilayer fashion. Smith-Petersen (extension), polysegmental, and pedicle subtraction osteotomies have all been used to treat fixed sagittal deformities. Many of these types of osteotomies were initially devised for the treatment of deformity secondary to ankylosing spondylitis and have been adapted to treat a variety of sagittal plane abnormalities, including flat back syndrome. The technique allows correction in both the sagittal and coronal planes of the spine. The spine is not lengthened, thereby avoiding the vascular and abdominal complications associated with extension osteotomies.
Syndromes
- Put your child to bed with a bottle of water only -- not juice, milk, or other drinks.
- Keep the person comfortable. The person should be rolled onto the left side, and remain there while getting or waiting for medical help.
- Magnetic resonance angiography (MRA)
- Infection in the brain, in the wound, or in the skull
- Aging changes in the kidneys
- Destruction of the mastoid bone
- Intestinal obstruction (blockage).
- Rapid, shallow breathing
The history offered by a patient with adjacent segment disease is often nonspecific and includes axial mechanical pain and complaints related to myelopathy or radiculopathy erectile dysfunction joliet cheap 20 mg cialis jelly amex. Characteristically, many patients with adjacent segment disease report a symptom-free interval, followed by the development of new progressive symptoms, in many cases several years after the index fusion procedure. Accordingly, detailed records from previous clinical evaluations should be reviewed and compared with the current symptomatology. Objective signs of a progressive neurological deficit, such as radiculopathy or myelopathy localizable to adjacent motion segments, are suggestive of adjacent segment disease. It is essential to note the presence of progressive changes in the neurological examination because many patients who have previously undergone fusion surgery harbor preexisting neurological deficits that are unrelated to the pathology of the adjacent spinal segments. Radiologic evaluation includes examination of both static and dynamic radiographs. These studies are invaluable for assessing the regional bony anatomy, for evaluating the integrity of the previous fusion construct, and importantly, for determining the presence of dynamic instability or a fixed spinal deformity of the adjacent motion segments. Information obtained from electromyography is also helpful in deriving objective evidence of nerve root dysfunction, which may arise from foraminal or lateral recess stenosis. A comprehensive synthesis of the information obtained from the history and neurological examination, imaging studies, and records of previous operations is required to formulate a detailed treatment plan. Indications for operative intervention include radiographic evidence of compression of neural elements with correlative signs of myelopathy or radiculopathy. Progressive or severe spinal deformity or mechanical instability and symptoms of axial mechanical pain are additional, but less common indications for operative intervention. The isolated presence of radiographically apparent adjacent segment degenerative changes may be monitored clinically. In these patients, the development of either radiculopathy, myelopathy, or symptomatic segmental instability may warrant surgical intervention. A trial of nonoperative therapy, such as epidural steroid injections, may benefit those with isolated radicular pain. Treatment the principles of treatment and the surgical goals of adjacent segment disease are similar to those of revision spine operations in general. In most cases of adjacent segment disease, decompression of the neural elements is the primary goal of surgery. Ancillary surgical goals include reduction of deformity, restoration of sagittal alignment, and stabilization. Stabilization and extension of the fusion are performed in the majority of patients rather than simple decompression. The surgical plan is largely influenced by the type of arthrodesis that was performed previously and by the nature and location of the neural element compression. Importantly, many of these patients harbor significant pathology at nonadjacent segments, and a more extensive decompression and fusion procedure is frequently required. Of paramount importance is avoidance of further mechanical destabilization and adjacent segment degeneration by preserving the adjacent supporting structures such as the facet joints, facet capsules, and interspinous ligaments. Comprehensive understanding of spinal biomechanics is essential in formulating an optimal surgical strategy that minimizes the risk for further adjacent segment degeneration and spinal deformity. Cervical Procedures Adjacent segment disease may occur after anterior or posterior cervical fusions. The location of the neural element compression and the type of arthrodesis that was performed previously largely dictate the choice of approach for a revision operation. After anterior fusion, ventral pathology of the adjacent segments, such as osteophytic spurs or disk herniations, should be directly addressed by performing ventral decompression and fusion. In patients with extensive ventral osseous compression, excellent results have been obtained by performing corpectomies followed by strut grafting and stabilization. Although a dorsal approach avoids the increased surgical risks associated with ventral cervical reoperations, it incurs the additional risks and morbidity associated with dorsal cervical surgery, such as axial pain, muscle denervation, and disruption of the posterior tension band. In cases in which neural element compression is incurred purely from dorsally located pathology, such as hypertrophic facet disease, dorsal decompression is indicated. Performance of a simple laminectomy without fusion for the treatment of cervical adjacent segment disease carries a risk for spinal destabilization and progressive kyphotic deformity.
Usage: q.2h.
The finding of multiple spinous process fractures is of greater concern in terms of the potential for instability impotence specialist order cialis jelly overnight. The specific role of imaging modalities, optimal timing of surgery, indications for surgery with some injury patterns, and the role of corticosteroids in the management of spinal cord injury are just a few areas that remain unresolved. Research into acute interventions to mitigate primary or secondary spinal cord injury continues, but without the prospect of a "silver bullet" emerging in the near future. As always, prevention of neurological injury before, during, and after the traumatic event is paramount for optimum outcomes. Functional recovery after decompressive spine operation for cervical spine fractures. Administration of methylprednisolone for 24 or 48 hours or tirilazad mesylate for 48 hours in the treatment of acute spinal cord injury. Results of the third National Acute Spinal Cord Injury Randomized Controlled Trial. Neurologic recovery following rapid spinal realignment for complete cervical spinal cord injury. Cervical spine fracture patterns mandating screening to rule out blunt cerebrovascular injury. Neurosurgical management of acute atlas-axis combination fractures: a review of 25 cases. Magnetic resonance imaging documentation of coexistent traumatic locked facets of the cervical spine and disc herniation. Cervical spine trauma associated with moderate and severe head injury: incidence, risk factors and injury characteristics. Cervical orthoses: a study comparing their effectiveness in restricting cervical motion in normal subjects. Atlanto-ocipital dislocation-part 2: the clinical use of (occipital) condyle-C1 interval, comparison with other diagnostic methods, and the manifestation, management and outcome of atlanto-occipital dislocation in children. Pediatric spine and spinal cord trauma: state of the art for the third millennium. The term, initially coined by Pang and Wilberger, referred to injuries that were most frequently described in children and resulted from the greater mobility of the pediatric osteoligamentous complex. A variety of mechanisms are seen, including hyperextension, flexion, flexion-extension, distraction, and direct crushing. The neurological deficits are frequently severe and result from cord transection or severe partial cord syndromes. In adults, such injuries were initially ascribed to hyperflexiondistraction with immediate reduction by muscular action or transient disk prolapse during forced flexion. ConcomitantVascularinjury the association of vertebral or carotid artery injury with cervical spine fractures is well known, although the incidence of such lesions remains controversial. Clearly, the anatomic relationship of the vertebral arteries and the cervical spine places these vessels at risk with fracture-dislocations and the like. Because these vascular injuries are often clinically inapparent, the incidence was formerly thought to be low. Several studies have reported rates of vertebral artery occlusive lesions of between 17. Recognition of injury and prevention of secondary or iatrogenic neurological injury are paramount considerations. A thorough understanding of injury patterns and clinical and radiographic manifestations is indispensable for accurate diagnosis and appropriate early management. The role of the neurological/spine surgeon is critical in directing the care of these patients, especially in the context of multiple trauma. One can expect craniocervical dissociation to account for about 1% of traumatic cervical spine injuries seen at an emergency treatment center. The extreme forces produced by hyperextension, hyperflexion, lateral flexion, or a combination of these forces lead to ligamentous failure. The first set attaches the skull to the atlas and includes the articular capsule ligaments, the anterior and posterior atlanto-occipital ligaments, and two lateral atlanto-occipital ligaments.
References
- Burch JC: Cooperis ligament urethrovesical suspension for stress incontinence, Am J Obstet Gynecol 100:764n774, 1968.
- Fucci C, Sandrelli L, Pardini A, et al: Improved results with mitral valve repair using new surgical techniques, Eur J Cardiothorac Surg 9:621-626, 1995, discussion 626-627.
- Gupta M, Lee MW: Treatment of stones associated with complex or anomalous renal anatomy, Urol Clin North Am 34:431n441, 2007.
- doi:10.1016/j.eururo.2018.
- Atkins D, Crawford F, Edwards J, et al: A systematic review of treatments for the painful heel. Rheumatology (Oxford) 38:968-973, 1999.
- Troppmann C, Gruessner AC, Sutherland DER, et al. Surgical complications requiring early relaparotomy after pancreas transplantation: a multivariate risk factor and economic impact analysis. Ann Surg. 1998;227(2): 255-268.
- The Writing Group for the PEPI Trial. Effects of estrogen or estrogen/progestin regimens on the heart disease risk factors in postmenopausal women. The Postmenopausal Estrogen/Progestin Interventions (PEPI) Trial. JAMA 1995; 273:199.
- Cooper CS, Chung BI, Kirsch AJ, et al: The outcome of stopping prophylactic antibiotics in older children with vesicoureteral reflux, J Urol 163(1):269-273, 2000.