Baclofen
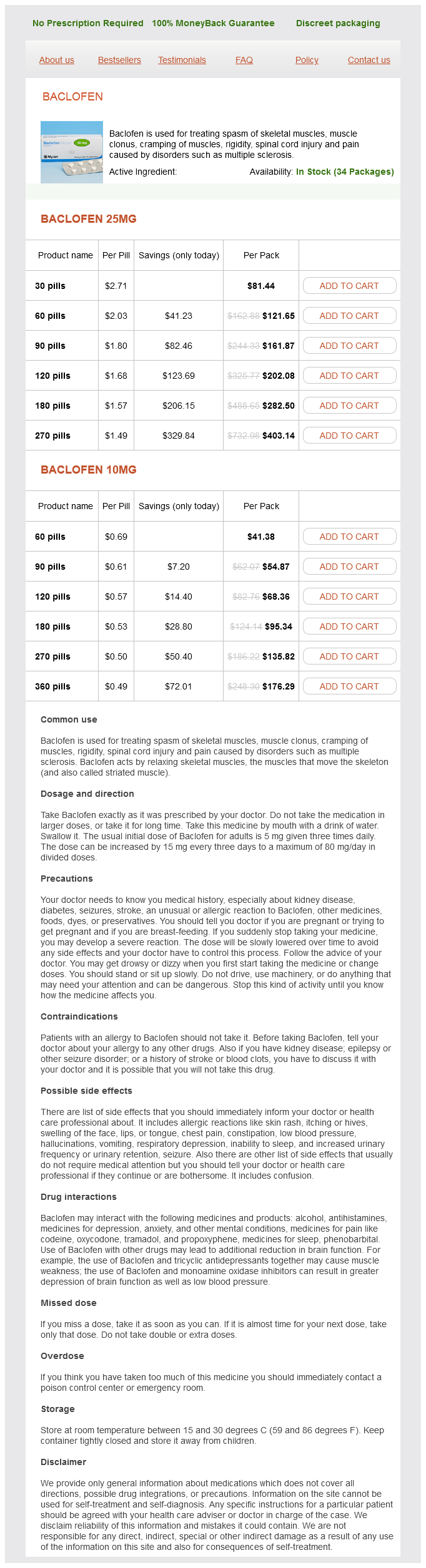
Baclofen 25mg
- 30 pills - $81.44
- 60 pills - $121.65
- 90 pills - $161.87
- 120 pills - $202.08
- 180 pills - $282.50
- 270 pills - $403.14
Baclofen 10mg
- 60 pills - $41.38
- 90 pills - $54.87
- 120 pills - $68.36
- 180 pills - $95.34
- 270 pills - $135.82
- 360 pills - $176.29
In addition muscle relaxant gabapentin purchase baclofen online now, because of its better safety profile, newer formulations of antifreeze also contain propylene glycol. Approximately 40% to 50% of administered propylene glycol is oxidized by alcohol dehydrogenase to both D-lactic acid and L-lactic acid. Considering that patients receiving many of the medications solubilized with propylene glycol frequently have other possible causes for their acidosis, it is important to be aware of this iatrogenic cause for the acidosis. Correction of the metabolic abnormalities quickly occurs following discontinuation of the medication. Unlike the lactate produced by glycolysis in animals, which is the L-isomer, colonic bacteria produce both the L-isomer and the D-isomer. Increased delivery of carbohydrates due to the shortened bowel and an overgrowth of bacteria is responsible for this overproduction. Mammalian clearance of D-lactate is far less efficient than that of L-lactate, and, with increased production within the gut, D-lactate accumulates within the blood. Because D-lactate is not detected on the routine assay, which measures only L-lactate, diagnosis requires a high clinical suspicion. Treatment consists of an oral fast with intravenous nutrition and restoration of gut flora to normal through the administration of oral antibiotics. In sepsis, restoring oxygenation with mechanical ventilation and perfusion with pressors or inotropes are of paramount importance, although these interventions do not always improve the lactic acidosis. In some patients with medicationinduced lactic acidosis, withdrawal of the offending agent may be sufficient. There are anecdotal case reports of successful use of riboflavin or L-carnitine to treat lactic acidosis associated with nucleoside analogues. Often these measures fail, and clinicians are faced with the decision of whether to give sodium bicarbonate in an effort to increase serum pH. First, as previously discussed, it is not clear to what extent acidosis is deleterious and therefore whether normalizing pH is of any benefit. Sodium bicarbonate is often given as a hypertonic solution, which can lead to hypernatremia and cellular dehydration. Thus it is difficult to recommend the use of bicarbonate for the treatment of a low serum pH alone. The protonated molecule is excreted by the kidney and should be used cautiously in patients with kidney failure. Potential side effects include hyperkalemia, hypoglycemia, ventilatory depression, and hepatic necrosis in neonates. The first 25% to 50% of the dose is given over 5 minutes and the rest over 1 hour. A large multicenter trial in humans showed a reduction in serum lactate, an increase in pH, and an increase in the number of patients able to resolve their hyperlactatemia. Despite these favorable changes, no improvement in hemodynamic parameters or mortality was found. Various modes of kidney replacement therapy have been used in the treatment of lactic acidosis. Standard bicarbonate hemodialysis treats acidosis primarily by diffusion of bicarbonate from the bath into the blood and is thus another form of bicarbonate administration, albeit with several advantages. Hypernatremia and volume overload are not a concern with bicarbonate administered via hemodialysis. Although the removal of lactate does not increase serum pH, there is some evidence that the lactate ion itself is harmful. Unfortunately, there are no randomized, prospective trials demonstrating the benefit of dialysis in lactic acidosis, and its use in the absence of other indications cannot be routinely recommended. Several studies have shown that high-volume hemofiltration using either lactate or bicarbonate buffered replacement fluid can rapidly correct metabolic acidosis. These studies have been small, and the degree and type of acidosis have been poorly characterized. In addition, other treatment measures have usually been instituted, making it difficult to draw conclusions about the effectiveness of this treatment. Although there are case reports of success using this modality, a randomized study comparing lactatebuffered peritoneal dialysis with continuous hemofiltration showed that hemofiltration corrected acidosis more quickly and more effectively than peritoneal dialysis. Whether newer bicarbonate-buffered peritoneal dialysis solution will be more efficacious remains unknown. Patients are generally polyuric and polydipsic, but if volume depletion becomes severe enough, polyuria may not be seen.
Baclofen dosages: 25 mg, 10 mgBaclofen packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
Enlarged lymph nodes should not be biopsied or opened as chronic sinuses will result muscle relaxant safe in pregnancy purchase baclofen 25 mg on line. Diagnostic Procedures: Complement fixation testing-80% of patients have a titer of 1: 16 or greater. Genital and lymph node specimens (ie, lesion swab or bubo aspirate) may be tested for C. Treatment should be started even before results of confirmatory tests are received. Patients should be advised to have all sexual partners examined for diagnosis and treatment. A review of the microbiology, immunology and clinical implications of Chlamydia trachomatis infections. Chancroid, lymphogranuloma venereum, granuloma inguinale, genital herpes simplex infection, and molluscum contagiosum. Mucocutaneous manifestations of chancroid, lymphogranuloma venereum and granuloma inguinale. Possible Complications: In one-third of patients, abscess formation, rupture, and fistula formation occur. Chronic progressive lymphangitis with chronic edema and sclerosing fibrosis may occur, causing extensive destruction of the vulva. Pregnant and lactating women should be treated with erythromycin (doxycycline use is contraindicated in pregnant women). Prevalence: 2/100,000; 1 of 4060 patients with gonorrhea; approximately 1% of all skin disorders in the United States. The appearance of lesions ranges from 1 week to 6 months, with an average incubation period of 6 weeks. Because patients who are immunosuppressed are at higher risk for molluscum, testing for Magnified view showing typical umbilicated lesion Keratin plug Inclusion bodies Histologic section of molluscum lesions showing pox virus inclusion bodies and central core of keratin Scattered distribution of molluscum lesions over perineum, buttocks, and thighs. Lesions spread by physical contact and autoinoculation Evaluation and management Application of liquid nitrogen to lesion using cotton swab with E. Special Tests: Material from the lesions is microscopically examined; inclusion bodies are seen in the material from the core of the lesion (molluscum bodies or Henderson-Paterson bodies). Expected Outcome: Good response to lesion destruction (generally heals with little or no scarring). A prospective randomized trial comparing the efficacy and adverse effects of four recognized treatments of molluscum contagiosum in children. Specific Measures: Molluscum lesions may go away on their own in 69 months but can persist, via autoinoculation, for up to 45 years. Curettage of the base of the lesion (with the tip of an 18-gauge needle or curette) is also curative. Comparison of 10% potassium hydroxide solution versus cryotherapy in the treatment of molluscum contagiosum: an open randomized clinical trial. The genome of molluscum contagiosum virus: analysis and comparison with other poxviruses. Scarring in Molluscum contagiosum: comparison of physical expression and phenol ablation. Treatment of multiple giant molluscum contagiosum in a renal transplant patient with imiquimod 5% cream. Description: Phthirus humanus (pubic or crab lice) and Sarcoptes scabiei (scabies or itch mite) are parasitic insects that may be transferred through sexual activity or contact with contaminated clothing or bedding. Scabies infections are not confined to hairy area but may be found in any area of the body. Scabies-bedding and clothing should be decontaminated (ie, either machine washed, machine dried using the hot cycle, or dry cleaned) or removed from body contact for at least 72 hours. Special Tests: Close inspection of the affected area generally reveals nits, feces, burrows, or the insects themselves. Diagnostic Procedures: History and physical examinations, microscopic examination of nits.
Chinese Mint (Japanese Mint). Baclofen.
- Dosing considerations for Japanese Mint.
- How does Japanese Mint work?
- Irritable bowel syndrome, itching, hives, mouth inflammation, rheumatic conditions, common cold, cough, fever, tendency to infection, nausea, sore throat, diarrhea, headaches, toothaches, cramps, earache, tumors, sores, cancer, cardiac complaints, sensitivity to weather changes, intestinal gas (flatulence), inflammation of the airways such as bronchitis, muscular pain (myalgia), ailments associated with nerve pain, and other uses.
- Are there safety concerns?
- What is Japanese Mint?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96610
In practice muscle relaxant carisoprodol buy 25 mg baclofen visa, most patients who develop severe hyperkalemia have multiple contributory factors. However, when he is started on indomethacin for acute gouty arthritis, the patient rapidly develops severe hyperkalemia. Hypokalemia also appears to increase the risk of ventricular arrhythmias in patients with ischemic heart disease or patients taking digoxin. Severe hypokalemia is associated with variable degrees of skeletal muscle weakness, even to the point of paralysis. There may also be decreased motility of smooth muscle, manifesting with ileus or urinary retention. Severe hypokalemia also interferes with the urinary concentrating mechanism in the distal nephron, resulting in nephrogenic diabetes insipidus. Such patients have a low urine osmolality in the face of high serum osmolality and are refractory to vasopressin. The correlation between serum potassium and total potassium deficit in hypokalemic patients is quite poor. Most diuretics (loop diuretics, thiazide diuretics, acetazolamide) increase urinary potassium excretion and tend to cause hypokalemia. However, potassium-sparing diuretics inhibit urinary potassium excretion and predispose to hyperkalemia by one of two mechanisms. Two other potassiumsparing diuretics, amiloride and triamterene, bind to the sodium channel in the collecting duct. This inhibits sodium reabsorption in the distal nephron and thereby limits the establishment of an electrochemical gradient required for potassium secretion. Interestingly, two antibiotics, trimethoprim (one of the components of Bactrim) and pentamidine, have also been shown to block the sodium channel in the collecting duct and therefore predispose patients to hyperkalemia. Because aldosterone plays an important role in enhancing renal potassium excretion in patients with kidney failure, drugs that inhibit aldosterone production (either directly or indirectly) predispose such patients to hyperkalemia. This effect occurs even with the low doses of subcutaneous heparin or enoxaparin used for prophylaxis of venous thrombosis in hospitalized patients. Tacrolimus, an immunosuppressant drug, may also cause hyperkalemia by inhibiting aldosterone synthesis. Given the stimulation of extrarenal potassium disposal by beta-adrenergic agonists, it is not surprising that beta-2 antagonists can predispose to hyperkalemia. There is significant systemic absorption of topical beta-blockers, and severe hyperkalemia may rarely be provoked by timolol eye drops. Drugs inhibiting endogenous insulin release, such as somatostatin, have been rarely implicated as a cause of hyperkalemia in patients with kidney failure. Presumably, long-acting somatostatin analogs, such as octreotide, would have a similar effect on serum potassium. Finally, drugs can also induce hyperkalemia indirectly by causing release of intracellular potassium from injured cells. Finally, the patient should be questioned about constipation, as the addition of laxatives may promote fecal potassium excretion. In normal individuals, the excess potassium is excreted in the urine such that the plasma potassium remains constant. In kidney failure, the potassium entering the extracellular fluid compartment during fasting cannot be excreted, thereby resulting in progressive hyperkalemia. The phenomenon of fasting hyperkalemia may be clinically significant in patients undergoing dialysis who fast longer than 8 to 12 hours before a surgical or radiologic procedure. Occasionally, such patients develop life-threatening hyperkalemia during a prolonged fast. The hyperkalemia can be prevented by the administration of intravenous dextrose (to stimulated endogenous insulin secretion) for the duration of the fast. If the patient is diabetic, insulin must be added to the dextrose infusion to prevent paradoxic hyperkalemia. If the patient has kidney failure, urgent dialysis is required for removal of potassium from the body. Because of the inevitable delay in initiating dialysis, the following temporizing measures must be initiated promptly: 1. The effect of 10 mL of 10% calcium gluconate solution over 1 minute is almost immediate.
Syndromes
- Any type of x-ray exam with dye (contrast material) within 3 days before the urine test
- AIDS patients
- Drawing a person with three parts
- Damage to the kidneys
- Unconsciousness or delirium
- Funnel-web spider venom
- Bleeding
- General discomfort, uneasiness, or ill feeling (malaise)
- Heart defibrillator or pacemaker
If nonabsorbable suture material is used to close the skin spasms movie 1983 baclofen 25 mg fast delivery, the stitches will need to be removed during a follow-up visit. Approximately 20% of breast biopsies in women age 50 are positive, and this figure increases to 33% in women aged 70 years or older. The majority of biopsies can be performed with curvilinear incisions following the contours of the breast, often in the circumareolar area. An open biopsy should be performed using a scalpel rather than electrosurgical energy because thermal effects on the biopsy material may blur the margin of normal tissue around the tumor and cause abnormally low receptor levels. The dissection is carried to the area of concern through a combination of sharp and blunt techniques. A change in tissue character or a "gritty" sensation may be noticed as the tissue is dissected near some mass lesions. The suture should not cause blanching of the tissue but should narrow the cervix so that it will not admit a single gloved finger. The tied suture should be both tied and cut in such a manner as to facilitate eventual location and removal. Based on the size of the cervix and needle chosen, it may be necessary to take additional suture passes to accomplish adequate circumferential support. Following conclusion of the procedure, the fetal heart rate is monitored to assure normal fetal status. Prophylactic antibiotics or -mimetic drugs have not been shown to be of any benefit in reducing the rate of complications or preterm labor. Some authors advocate prescribing a non-steroidal anti-inflammatory drug, such as indomethacin, for the first 1224 hours after cerclage placement, but data are conflicting and the effects small. When the suture is to be removed (generally at 38 weeks and always if labor ensues before that time), it may be carried out in the office or labor and delivery area by firmly grasping the knot or visible suture ends and applying traction to identify one side of the suture below the knot. Snipping this portion of the suture allows traction on the knot to pull the suture through the tissues for removal. An anesthetic may be required based on exposure, patient comfort, and provider or patient preference. Cervical cerclage is the placement of a suture or tape to support and partially occlude the uterine cervix to reduce the risk for preterm delivery in the face of cervical insufficiency. A number of procedures have been described, but the most common and simplest is the McDonald cerclage, which is described here. Cervical cerclage may also be accomplished by placing the suture via an abdominal route, although this is a much more invasive procedure and the suture is generally left in place permanently, precluding vaginal delivery. Cerclage may be placed based on history or cervical shortening documented through ultrasonography. Prophylactic cervical cerclage is generally delayed until after 14 weeks so that early pregnancy losses from other factors may be resolved. Beyond 2426 weeks, bed rest, pessary therapy or other treatments are often preferred because of the increased risk for surgically related labor. Scarring from the procedure may lead to cervical lacerations during labor (1%13%) or failure of the cervix to dilate (2%5%). Any obvious vaginal or cervical infections should be treated, and cultures for gonorrhea, chlamydia, and group B streptococci should be obtained prior to proceeding. Sexual intercourse is generally proscribed for 1 week before and after the procedure. The anesthetized patient is placed in the dorsal lithotomy position, the vagina and cervix are disinfected, and the cervix is visualized using retractors. When the suture is placed vaginally, it is generally removed at 38 weeks of gestation. Cervical Incompetence Prevention Randomized Cerclage Trial: Emergency cerclage with bed rest versus bed rest alone. Cerclage for prevention of preterm birth in women with a short cervix found on transvaginal ultrasound examination: a randomized trial. Randomised trial of cervical cerclage, with and without occlusion, for the prevention of preterm birth in women suspected for cervical insufficiency. Multicenter randomized trial of cerclage for preterm birth prevention in high-risk women with shortened midtrimester cervical length.
Usage: q.2h.
Activation of the alternative pathway of complement by monoclonal lambda light chains in membranoproliferative glomerulonephritis spasms near sternum 25 mg baclofen sale. Dense deposit disease: clinicopathologic study of 32 pediatric and adult patients. Primary glomerulonephritis with isolated C3 deposits: a new entity which shares common genetic risk factors with haemolytic uraemic syndrome. Heterogeneous pattern of renal disease associated with homozygous factor H deficiency. Epidemiology, clinical presentation, and pathophysiology of atypical and recurrent hemolytic uremic syndrome. In cases of ongoing active infection, other clinical manifestations related to the specific infectious disease are common. Sites of infection can include the upper and lower respiratory tract, skin/soft tissue, bone, teeth/oral mucosa, heart, deep abscesses, shunts, and indwelling catheters. Adults more commonly present with kidney failure and with complications of hypervolemia, including decompensated heart failure. In these cases, coexistence of the glomerular disease and the infection is common, and classic clinical findings such as low complement levels may be absent. Diabetes is the most commonly recognized comorbidity and is associated with poor outcomes. The presentation and outcomes in children are often different from those in adults (Table 22. The urinary sediment is usually active, with dysmorphic red cells, red blood cell casts, and leukocyturia. Hypocomplementemia is very common, with decreased C3 in up to 90% of cases and to a lesser extent depleted levels of C4. There is usually a "latent" period between the resolution of the streptococcal infection and the acute onset of the nephritic syndrome. This period is usually 7 to 10 days after oropharyngeal infections and 2 to 4 weeks after skin infections. Elevation of these four markers has a yield of approximately 80% in documenting recent streptococcal infection. A diffuse endocapillary proliferative and exudative (neutrophil-rich) glomerulonephritis ([A] hematoxylin and eosin, 400× magnification) is the most common pathology encountered in infection-related glomerulonephritis. A membranoproliferative pattern ([B] Jones methenamine silver stain, 400× magnification) with large subendothelial immune deposits can be seen in cases where infection is long-standing, such as in shunt nephritis. Underlying chronic diseases, such as diabetic nephropathy, may exist and modify the appearance of glomeruli. Deposits are typically C3 dominant or co-dominant and accompanied by immunoglobulin staining of lesser intensity. The "garland pattern" of C3 staining is illustrated in (B) (600× magnification) and more clearly demonstrates the contour of the glomerular basement membrane, because subepithelial deposits are in abundance and nearly confluent. The staining in (D) is for IgA (400× magnification), and a nodular, largely mesangial distribution of positive staining can be seen. Immunofluorescence typically shows dominant or codominant staining for C3, usually accompanied by lesser degrees of immunoglobulin staining. In staphylococcal infections, IgA is commonly the dominant immunoglobulin, and in up to 25% of cases, the C3 is not associated with significant amounts of immunoglobulin staining. Subendothelial deposits, though often less pronounced, are largely responsible for the prominent endocapillary proliferation that is often seen. IgA nephropathy, because of its synpharyngitic presentation, is also frequently considered in the differential diagnosis. A combination of serologic testing and features on kidney biopsy can help distinguish these entities, but pitfalls exist. It is the typically smaller subendothelial deposits (arrow) that are likely responsible for producing much of the diffuse proliferative changes usually seen by light microscopy. In these cases, evaluation for abnormalities of the alternative complement pathway should be considered.
References
- Touijer KA, Karnes RJ, Passoni N, et al: Survival outcomes of men with lymph node-positive prostate cancer after radical prostatectomy: a comparative analysis of different postoperative management strategies, Eur Urol 73(6):890n896, 2018.
- Doroshenkova AE, Grebennikov S, Kozhemyakin A, et al. Primary and repeated operations in surgery of TB. VII Congress of the Russian Phthisiatricians: Tuberculosis Today, 2003; Abstract P277.
- Gear JSS, Ware A, Fursdon P, et al. Symptomless diverticular disease and intake of dietary fibre. Lancet 1979;i:511.
- Caraballo RS, Shafer PR, Patel D, et al. Quit methods used by US adult cigarette smokers, 2014-2016.
- Meijboom WB, Mollet NR, Mieghem CAV, et al: 64-slice CT coronary angiography in patients with non-ST elevation acute coronary syndrome. Heart 2007;93:1386-1392.
- Moran GJ, Barrett TW, Mower WR, et al: Decision instrument for the isolation of pneumonia patients with suspected pulmonary tuberculosis admitted through US emergency departments. Ann Emerg Med 53:625-632, 2009.
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness. a practical scale. Lancet. 1974;2:81-84.
- Rotthier A, Baets J, De Vriendt E, et al. Genes for hereditary sensory and autonomic neuropathies: A genotype-phenotype correlation. Brain. 2009;132(Pt 10):2699-2711.